Case Report
Preserved Scleral Patch Graft for Scleral Thinning in a Repaired Ocular Trauma: A Case Report
Neeti Gupta*, Kanishk Singh, Renu Dhasmana , Amit Maitreya, Harsh Bahadur, R C Nagpal
Corresponding author: Dr. Neeti Gupta, Assistant Professor, Department of Ophthalmology, Himalayan Institute of Medical Science Swami Ram Nagar, Jolly Grant, Doiwala, Dehradun, Tel.: 0135-2471440, Fax: 0135-2471317, India,; E-mail: drneetigupta@rediffmail.com
Citation: Gupta N, Singh K, Dhasmana R, Maitreya A, Bahadur H, et al. Preserved Scleral Patch Graft for Scleral Thinning in a Repaired Ocular Trauma: A Case Report. Indian J Ocular Biol. 2015;1(1): 101.
Copyright © 2015 Neeti Gupta et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Submission: 12/01/2015; Accepted: 24/02/2015; Published: 28/02/2015
Abstract
Introduction
Human scleral grafts are widely used for covering scleral thinning in ophthalmic surgery. Case: A 28-year-old male presented with traumain the right eye by an iron piece. A 10mm scleral perforation was seen 2mm behind the limbus, with uveal incarceration along the perforation site. A primaryrepair of the laceration was done followed by applying a glycerol preserved scleral patch graft over wound site. The focus of this report is on method used aswell as the material for the repair in tertiary care center.
Conclusion
Allogenic scleral grafting is an effective and simple measure for preserving globe integrity both structurally and functionally.
Keywords: Penetrating injury; Scleral patch graft
Introduction
Human sclera grafts are widely used in ophthalmic surgery. They are mainly used for scleral perforation repair [1], covering scleral thinning as in scleromalacia [2] or in reconstruction after complicated filtering bleb surgery in glaucoma like leaking or overfiltering bleb [3,4], eyelid reconstruction [5] and exposed hydroxyapatite orbital implants [6]. We report an interesting case of repaired ocular trauma of a young male, where bulging of the wound site due to raisedintraocular pressure, was managed by applying a scleral patch graft.
The Case
A 28-year-old male presented with a history of trauma in the right eye by iron piece in May 2012. On examination the best corrected visual acuity was PL positive with PR accurate in all quadrants in right eye and 20/20 in left eye. On slit lamp examination a scleral laceration was seen about 2mm behind the limbus, with uveal incarceration along the perforation site. Hyphema was present in the anterior chamber along with iridodialysis. Posterior segment could not be visualized due to vitreous haemorrhage. CT Scan of the orbit showed no intraocular foreign body. According to the Bermingham ocular trauma scale the injury was classified as Zone 3, Type 2, Grade 4,RAPD absent [7].
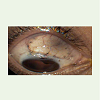
On exploration under general anesthesia the laceration was found to be 10 mm in size about 2mm behind the limbus , passing through the insertion of the superior oblique muscle. A primary repair of the laceration was done with 6-0 silk suture after disinsertion of Superior Oblique muscle, which was again reinserted with 6-0 vicryl at its previous insertion site on the sclera. Hyphaema drainage was also done and patient was kept on topical and oral steroids along with topical antibiotics. On follow up after 3 weeks, BCVA of the patient was 20/40, Anterior chamber was well formed with a D shaped pupil normally reacting to light and intraocular pressure was 28mm of Hg by goldmann applanation tonometer. Bulging of uveal tissue was seen through the weakened sclera due to raised IOP (Figure 1).The posterior segment was normal with mild vitreous haemorrhage in the inferior quadrant (Figure 2).
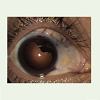
The patient was managed by applying glycerol preserved scleral patch graft over wound site. The donor sclera was obtained from the eye bank preserved in glycerol. This donor sclera was first rehydrated by immersing the tissue in balanced salt solution for 15 minutes to which antibiotic was previously added. Then 15×15mm donor sclera was cut and sutured over the recipient bed with 8-0 nylon suture and was then covered with conjunctiva. The patient was kept on pressure lowering agents. After 1 month post surgery the vision of the patient improved to 20/20 and the scleral patch graft has been well taken up with IOP of 18 mm of Hg by AT on topical dorzolamide and timolol (Figure 3 and Figure 4). In recent follow up (10 months) the vision of the patient is 20/20 with a healthy sclera graft.
Discussion
Scleral thinning is a well reported complication following ocular trauma repair, pterygium excision [8], retinal detachment repair, systemic vasculitis [9] and high myopia [10]. Reinforcement of thin or perforated sclera is necessary to prevent prolapse of ocular contents and secondary infections, especially in the case of choroidal exposure. Different tissue like fascia lata, cartilage, tibial periosteum, cadaveric aortic tissue, amniotic membrane, Gore-Tex, autologous and homologous sclera have been successfully used as graft for managing sclera defect and tectonic instability of eye [9,2]. Autologous preserved sclera patch graft has several advantages as proposed to other grafts, as scleral tissue is easily available from whole eye donors which can be preserved for months, is strong and flexible, has natural curvature of sclera allowing better fit to host defect and easy to handle. Donor sclera is well tolerated by host with little inflammatory reaction and rare rejection. However to avoid complication like necrosis and melting of graft dehiscence and post operative endophthalmitis, the avascular sclera patch graft must undergo epithelization and vascularization which is stimulated with conjunctiva covering, a free conjunctival flap or an amniotic membrane graft [11]. The only criticism of use of sclera is that it may become involved in the ongoing necrotic process or being avascular may melt. In our case, the precipitating factor for sclera thinning and uveal tissue bulging was repaired scleral perforation and increased IOP. In this case after applying sclera patch, graft was covered by conjunctival flap to prevent its necrosis and sloughing and favorable structural and visual outcome was achieved postoperatively.
Conclusion
Allogenic scleral grafting is an effective and simple measure for preserving globe integrity both structurally and functionally. Scleral weakening along with bulging of the uveal tissue was successfully managed with application of a scleral patch graft along with lowering of IOP.
References
- RodrigueZ-Ares MT, Tourino R, Capeans C, Sanchez-Salorio M (1999) Repair of sclera perforation with preserved sclera and aminotic membrane in Marfan’s syndrome. Ophthalmic Surg Lasers 30: 485-487.
- Oh JH, Kim JC (2003) Repair of scleromalacia using preserved scleral graft with amniotic membrane transplantation. Cornea 22: 288-293.
- Harizman N, Ben-Cnaan R, Goldenfeld M, Levkovitch-Verbin HJ, Melamed S (2005) Donor sclera patch for treating hypotony due to leaking and/or overfiltering blebs. J Glaucoma 14: 492-496.
- Kosmin AS, Wishart PK (1997) A full-thickness sclera graft for the surgical management of a late filtration bleb leak. Ophthalmic Surg Lasers 28: 461-468.
- Kamiya H, Kitajima Y (2003) Successful use of preserved sclera of eyelid reconstruction. Eur J Dermatol 13: 267-271..
- Inkster CF, Ng SG, Leatherbarrow B. Primary banked sclera patch graft in the prevention of exposure of hydroxyapatite orbital implants. Ophthalmology 2002;109(2):389-92. Comment in Ophthalmology 2003;110(7):1281; author reply 1281. Ophthalmology. 2003;110(7):1282:author reply 1282.
- Kuhn F, Morris R, Witherspoon CD (2002) Birmingham eye trauma terminology : terminology and classification of mechanical eye injuries. Ophathamol clin north Am 15: 139-143.
- Alsagoff Z, Tan DT, Chee SP (2000) Necrotising scleritis after bare sclera excision of pterygium. Br J Ophthalmol 84: 1050-1052.
- Nguyen QD, Foster CS (1999) Scleral patch graft in the management of necrotizing scleritis. Int Ophthalmology Clin 39: 109-131.
- Bosley WE,Synder AA (1958) Surgical treatment of high myopia. Trans Am Acad Ophthal Otolaryngol 62: 791-802.
- Stunf S, Lumi X, Drnovsek-Olup B (2011) Preserved scleral patch graft for unexpected extreme scleral thinning found at scleral buckling procedure. Ind J ophthalmol 59: 235-238.