Research Article
Seizure Outcome Relates to Prognostic and Histological Factors in Patients with FCD and HS Associated Partial Epilepsy
Pradeep Madhamanchi1,2, Sujatha Peela3, SPD Ponamgi4, Kishore Madhamanchi1, Jayalakshmi S5, Manas P5, Madhavarao Panchareddi3, and Prakash Babu P1*
1Department of Biotechnology and Bioinformatics, University of Hyderabad, Gachibowli, Telangana, India
2Department of Biotechnology, Dr. B. R. Ambedkar University-Srikakulam, Andhra Pradesh, India
3Centre for Applied Sciences, Government Degree College (Men)-Srikakulam, Andhra Pradesh, India
4Department of Neurology, Krishna Institute of Medical Sciences, Secunderabad, India
2Department of Biotechnology, Dr. B. R. Ambedkar University-Srikakulam, Andhra Pradesh, India
3Centre for Applied Sciences, Government Degree College (Men)-Srikakulam, Andhra Pradesh, India
4Department of Neurology, Krishna Institute of Medical Sciences, Secunderabad, India
*Corresponding author: Prakash Babu Panithi, Department of Biotechnology and Bioinformatics, University of Hyderabad, Gachibowli, Telangana, India. E-mail Id: prakash@uohyd.ac.in
Article Information: Submission: 28/08/2023; Accepted: 14/09/2023; Published: 17/09/2023
Copyright: © 2023 Pradeep Madhamanchi, et al. This is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Focal Cortical Dysplasia (FCD) and Hippocampal Sclerosis (HS) patients often present with seizures or pits which are drug resistant in nature. These patients can be seizure-free after lesion resection. However some still experience seizures after surgery. The present study aimed to analyze the clinical data
of a group of FCD and HS allied partial epilepsy patients and evaluate their seizure outcomes and prognostic factors. Follow-up study involved clinical data collected from medical records of patients diagnosed with FCD and HS pathologically and underwent surgical resection in Department of Neurology, Krishna
Institute of Medical Sciences (KIMS), Secunderabad. The seizure outcomes were evaluated based on the International League against Epilepsy (ILAE) classification. The prognostic factors were identified according to univariate and multivariate analysis. A total of 576 (FCD = 174; HS = 402) patients were
included, with a mean age at surgery of 17.32 ± 8.34 years for FCD and 10.74 ± 7.24 years for HS. All patients were followed up at least for one year with a
mean follow-up duration of 7.98 ± 3.84 years. At the final follow-up, 89 (51.6%) of FCD and 324 (80.5%) of HS patients achieved ILAE Class 1 or 2. Univariate and multivariate analyses revealed that the short duration of seizures and gross total resection were significant positive factors for seizure-free. Bilateral
interictal or ictal epileptiform discharges in preoperative video-electroencephalogram (VEEG) were related to poor seizure outcomes. Surgical resection is an effective treatment for patients with FCD and HS-associated partial epilepsy. The analysis of predictive factors could effectively guide clinical practice and
evaluate the prognosis of drug-resistant epilepsy.
Keywords: Focal Cortical Dysplasia; Hippocampal Sclerosis; Partial Epilepsy; Surgical Resection; Seizure Outcome; Prognostic Factors
Introduction
Epilepsy is the condition where spontaneous recurrent seizures
happening and it is the major neurological disorders, with a prevalence
of 6.38 % -7.60 % [1]. In the series of epilepsy surgery, FCD and HS
of the CNS graded as the most common class of pathology leading to
epilepsy with drug resistance [2]. Brain respective surgery is an efficient
treatment for focal epilepsies with drug resistance of seizure freeness
ranging from 60 % to 80 % within 01 % to 02 % follow-up years, 40
to 50 at 10 years of follow-up [3]. Added advantages in surgery are
increased expectancy of [4], decreased sudden death risk [5], better life quality [6], mood improvement and regain of cognitive function
[7]. All in all, these upshots are much better to the other choices of
ablation, neuro modulation, and/or current medical therapy [3]
Nevertheless, almost 1/3 of patients persist to have convulsions after
surgery, besides the resultant long term outcome is poorer than the
immediate outcome, with 48% to 58% experience seizures continuing
after 5 years of surgery [8,9]. Hence it is urgency to reliable surgical
outcomes predictors for HS and FCD linked epilepsies and choosing
proper surgical patients remains a defy [10]. Some studies reported
the threat reasons for postoperative surgery outcomes, but a section
of these studies concentrated only on definite populations or on site
specific focal lesions such as FCD and HS. Added to it, few articles
reported only HS and FCD as a segment of the study object. In
addition, previous results of research had only a certain worth to
direct clinical work, as the research done with limited sample sizes.
Herein, we studied a case strings engaging a total of 576 (FCD = 174;
HS = 402) partial or focal epileptic patients to describe the clinicohistological
characteristics and assess the outcome of surgery and
predictors of prognosis. As per our familiarity, the current study is the
largest group in the single study center.
Materials and Methods
Selection of Patients:
This one institution study was agreed by the local committee of
ethics. The criteria of inclusion were:
[i] Patients joined to Neurology Department, KIMS, Secunderabad
from February 2010 to January 2018
[ii] Postoperatively confirmed the existence of FCDs and HS.
The rulings out criteria were:
[i] No seizures
[ii] A history of previous surgery
[iii] Clinical, electrophysiological, neuro radiological and
pathological data not available to review
[iv] No surgical resection in patients
[v] Patients who lost during postoperatively. Medical records of
patients’ were reviewed retrospectively for detailed demographic,
histological, clinical variables. The focal epilepsies allied with FCD
and HS were classified according to the ILAE [11].Pre-operative assessment:
All patients subjected to non-invasive tests, including usual pre
surgical valuations, such as detailed history, seizure semiology, brain
MRI, neurological examination and long-term VEEG. MRI scans
comprised T1-, T2- and FLAIR images. The lesion changes and
epileptic site were analysed by neuro radiologist. The electrodes placed
as per the standard 10 to 20 system with long-term 64 channels VEEG
monitoring. IEDs or inter-ictal epileptiform discharges were named:
a. Regional - IEDs involved 1 lobe or adjacent lobes; b. Unilateral -
IEDs generated at ipsilateral hemisphere of the FCD or HS; c. Bilateral
– IEDs in both hemispheres. Recorded ictal seizures from the patients
were classified as a. Regional, b. unilateral and c. bilateral as per the
IEDs. Neurologists and Electro physiologists teamed to spot the EZ
(epileptogenic zone) depending on the observations of semiology
and VEEG. Classification of seizure type was depending on the
ILAE 2017 version [12]. Epilepsy surgery suitability was confirmed
by a series of pre surgical examinations by a multi-disciplinary panel
comprises of electro physiologists, neuro radiologists, neurosurgeons,
and neurologists. In case the patient’s VEEG depicted as the IEDs
was localized and steady with the neuro imaging findings and
symptomatological, usually the patient could directly proceed to the
surgical stage. Other cases, patients require going into the 2nd stage of
valuation.Some particular non-invasive examinations need to be performed:
1. Magneto encephalography or MEG
2. Positron Emission Tomography-Computed Tomography or
PET- CT. The EZ can be determined by non-invasive assessment in
majority of the patients having FCD and HS. However in some patients
the preoperative evaluation showed that the EZ was incompletely
reliable with the lesion. In such cases, depth electrodes or subdural
grids were implanted robotically to find the EZ.
Surgery procedure:
The ultimate aim of surgery was the gross sum resection of the
EZ with minimal or no complications. Neuro monitoring facilities
like Intra-operative electro corticography or ECoG were conducted
to define the EZ and found the functional regions. The surgical form
was defined like: 1. GTR: No residual FCD or HS tissue identified on
postoperative MRI
2. NTR: > 90% of the FCD/HS tissue was resected
3. STR: < 90% of the FCD/HS tissue was resected. Pathologists
confirmed histopathology reports revealed that the tissues had an
emblematic structure of FCD and HS.Seizure Upshot during Follow-Up:
All the patients who have undergone surgery for epilepsy were
followed by the neurosurgeon in every 2 months at outpatient in the
first year and annually after that. Scalp EEG and MRI were essential to
find whether the EZ completely resected in all the patients at the 1st reexamination.
The seizure upshots were recorded on far with the ILAE
system for seizure outcome [13] with favorable or good outcomes
defined as Class-I; unfavorable or poor outcomes as class-II-VI. All
the patients resumed to get AEDs as prophylaxis post-surgically. EEG
results and patients’ surgery outcome decided whether to wean off
or lessen the amounts of AEDs after surgery. Monotherapy patients
would be able to wean off AEDs after the sugary gradually, if they:
i. No convulsions for two years; ii. No IEDs in EEG; iii. No FCD/
HS lesions reappearance on MRI. Polytherapy Patients who met the
above necessities could slowly reduce the dose of AEDs. Otherwise,
the AEDs therapy should be planned as per the patients’ test results.Statistical Analysis:
For the continuous variables, means, ranges and SD are
represented. Frequencies and % are presented for definite data. The
definite or categorical data was analysed by Fisher’s z-test or Pearson
X2 test. Multivariate and/or univariate analyses were done to find the
seizure outcome predictors. All statistical studies were performed
with the SPSS software version 25 (IBM). P-value <0.05 is statistically
significant.Results
Demographic Details:
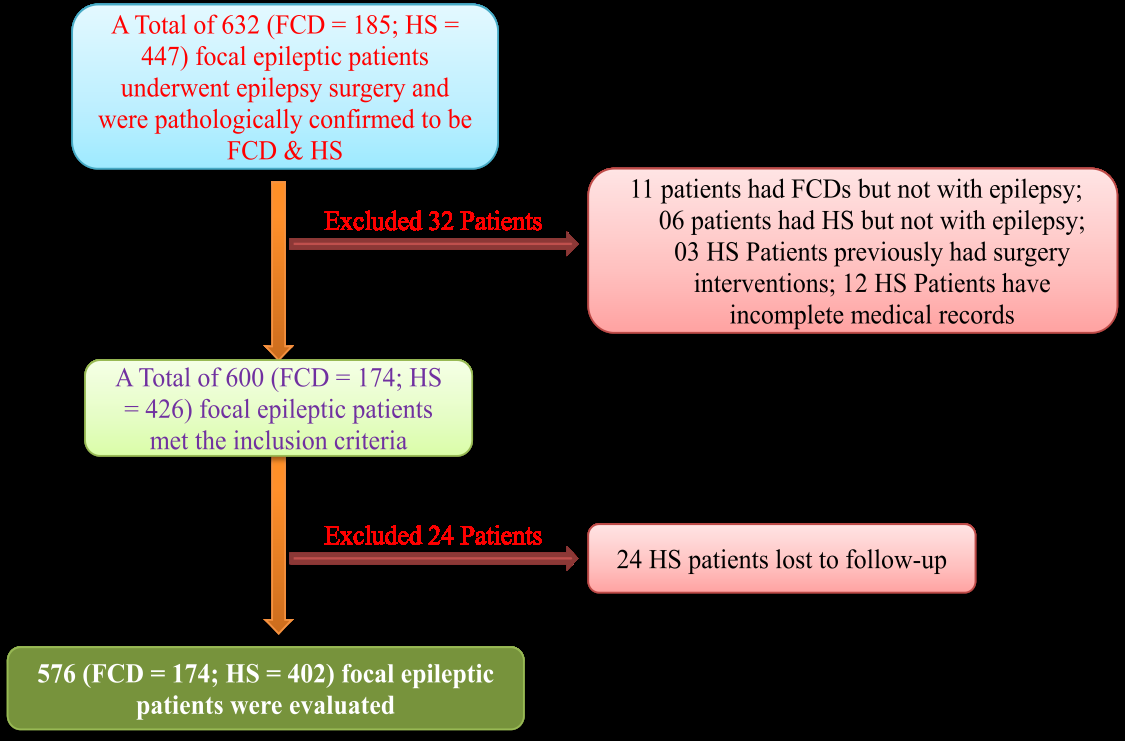
During February 2010 to January 2018, 576 (FCD = 174; HS =
402) patients (109 males and 65 females in FCD; 287 males and 115
females in HS) qualified the criteria of inclusion and enrolled for
study. At the time of surgery, the average age was 17.32 ± 8.34 years
for FCD and 10.74 ± 7.24 years for HS (Range: 1.5 – 67.0 for FCD;
1.2 – 69.0 for HS), the seizure onset average age was 11.54 ± 6.37 Y for
FCD and 9.11 ± 7.17 Y for HS (Range: 1.0 – 65.0 for FCD; 0.9 – 67.0
for HS), seizures average duration was 5.78 ± 7.28 (where range = .1–
20.3) Y for FCD and was 5.1 ± 6.8 (range, 0.1– 18.3) years for HS. The
process of patient-selection was showed in [Figure 1].Clinical Characteristics:
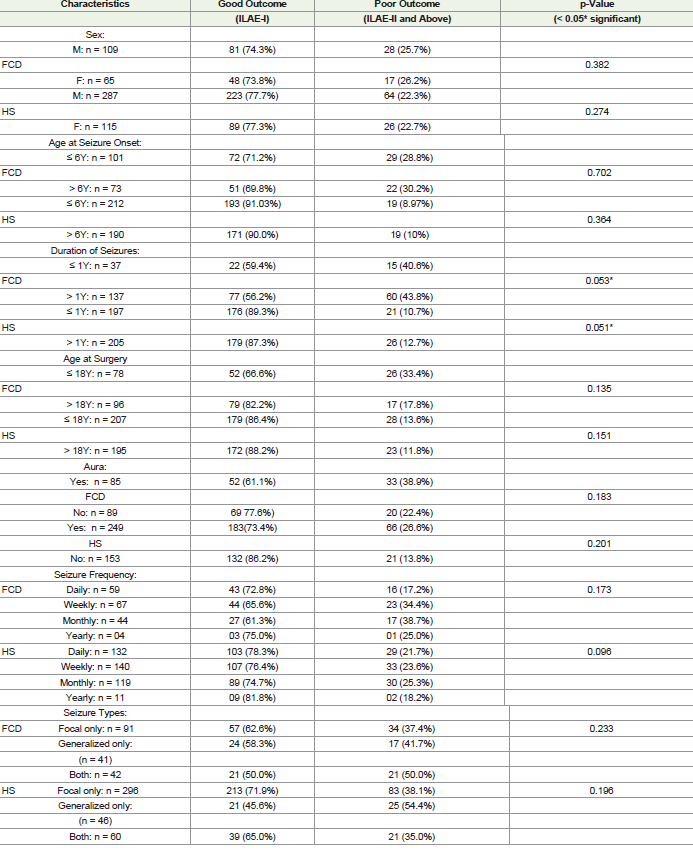
[Table 1] presented clinical individualities of all patients,
depicting that 334 (FCD: 85+HS: 249 = 57.9%) patients experienced
an aura prior to the seizures. The seizure onset was recorded every
day (daily) in 191 (FCD: 59+HS: 132 = 33.1%), weekly in 207 (FCD:
67+HS: 140=35.9%), monthly in 163 (FCD: 44+HS: 119=28.2%), and
yearly in 15 (FCD: 4+HS: 11=2.8%) patients. In the cohort, 387 (FCD:
91+HS: 296=67.1%) had only focal-onset seizures, 87 (FCD: 41+HS:
46=15.10%) only had onset of generalized seizures, and the rest of the
patients 102 (FCD: 42+HS: 60=17.7%) had duel seizure types. Sixty
one (FCD: 26+HS: 35=10.6%) patients had no AEDs before surgery,
perhaps due to the squat duration of epilepsy or the less frequency of
seizures, 117 (FCD: 37+HS: 80=20.3%) were underwent monotherapy
and 398 (FCD: 111+HS: 287=69.09%) patients undergone polytherapy.
At the end of the follow-up, 123 (FCD: 41+HS: 82) of the 576 (21.3%)
patients weaned off AEDs, 301 (FCD: 47+HS: 254=52.2%) patients
underwent monotherapy, and the rest 152 (FCD: 86+HS: 66=26.3%)
were still accepting polytherapy. The average AED number after
surgery (0.99 ± 1.08) was greatly lesser than at baseline (3.56 ± 0.87)
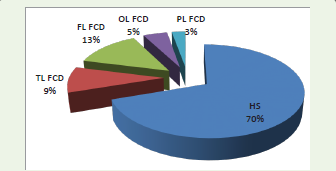
(P < 0.005).All the patients had preoperative examination of MRI. HS in TL
identified in 402 (69.7%) individuals. Patients with FCD located in
TL, FL, PL and OL were found in 53 (9.2%), 77 (13.3%), 16 (2.7%) and
28 (4.8%) respectively [Figure 2].
Figure 2: Location distribution of HS & FCD; Frontal lobe = FL; Temporal
lobe = TL; Parietal lobe = PL; Occipital lobe = OL
To all patients, scalp EEG checking results were obtained. Regional
IEDs found in 372 (FCD: 74+HS: 298 = 64.5%) patients, unilateral in
123 (FCD: 51+HS: 72 =21.3%), and bilateral in 81 (FCD: 49+HS: 32
=14.06%). Regional ictal onset rhythms found in 385 (FCD: 101+HS:
284 =66.8%), unilateral in 135 (FCD: 41+HS: 94 = 23.4%) and bilateral
in 56 (FCD: 32+HS: 24 = 9.7%) individuals. The seizures onset could
not captured due to insufficient time for monitoring of EEG in 93
(FCD: 22+HS: 71 = 16.1%) individuals. For precise localization of
EZ, 398 (FCD: 125+HS: 273 =69.09%) patients underwent MEG, 141
(FCD: 41+HS: 100 =24.4%) underwent PET-CT, and 37 (FCD: 8+HS:
29 =6.4%) underwent intracranial electrode implantation. GTR of the
focal lesion (FCD or HS) was achieved in 347 (FCD: 81+HS: 266 =
60.2%) cases, NTR was attained in 171 (FCD: 53+HS: 118 = 29.6%),
and STR was achieved in 58 (FCD: 40 +HS: 18 = 10.06%) individuals.
Histopathological records disclosed that the collected tissue samples
had a representative structure of FCDs and HS. A total of 174 (FCDIA:
25+FCD-1B: 31+FCD-IIA: 57+FCD-IIB: 36+FCD-III: 25 =
30.2%) were classified as various types of FCDs and the rest 402 were
TLE-HS patients.
Surgical Difficulties:
During this case strings, at the final follow-up no patient lost by
seizure recurrence. A total of 96 (FCD: 61+HS: 35=16.6%) individuals
had transitory neurological complications which did not influence
their life quality, consist of 24 (FCD: 16+HS: 8=4.1%) with muscle
weakness, 34 (FCD: 23+HS: 11=5.9%) with contra lateral quarterquadrant
hemianopia, 15 (FCD: 06+HS: 11=2.6%) with memory
impairment, 8 (FCD: 05+HS: 03=1.3%) with transient dysphasia, 5
(FCD: 04+HS: 01=0.8%) with intracranial infection, 3 (FCD: 02+HS:
01=0.5%) with wound infection, and 6 (FCD: 04+HS: 2=1.04%) with
CSF outflow. After comprehensive treatment, all 96 patients revisited
to work or study. Added to it, 103 (FCD: 81+HS: 22=17.8%) patients
suffered permanent neurological deficits, 43 (FCD: 31+HS: 12=7.4%)
had hemi paresis, 18 (FCD: 11+HS: 07=3.1%) had facial paresis,
11 (FCD: 06+HS: 5=1.9%) had dysphasia, including 2 FCD (0.3%)
patient with motor aphasia and 5 FCD (0.8%) patients with sensory
aphasia, 3 FCD (0.5%) patients had hemianopia, and 1 HS (0.17%)
patient with paresthesia. Even though the patients were subjected to
postoperative healing training, they remain had signs that threaten
their lives. It would be understand that the malfunction presented
prior to treatment was excluded in the surgical impediments.
Table 1: C linical, Demographic & Histological personalities of patients with focal epilepsies and association with surgery outcomes
Outcome During Follow-Up:
24 individuals went for reoperation. Fifteen of them subjected to
FCD lesion deletion based on CT observations. Remaining 9 patients
underwent HS removal that overlapped with functional areas.
Ultimately, all of them achieved seizure-free, but 4 (FCD: 2 and HS: 2)
of them had sensory aphasia and hemi paresis observed in two FCD
individuals. At least for 1 Y, all the individuals were followed up with
an average observation span of 7.98 ± 3.84 years. At the final followup,
89 (51.6%) of FCD and 324 (80.5%) of HS individuals achieved
ILAE-I and II. Uni and multivariate analysis disclosed that the less
span of seizures and GRT were significant supportive reasons for
seizure-freeness. Among the 576 sufferers, 54 had convulsions only
one time or rare auras even after missing of AEDs, included in the
favorable outcome group.Predictive Causes:
The possible predictive factors allied with seizure upshot by
univariate analysis were as follows:
Seizures duration (FCD: P = 0.053; HS: P = 0.051), IEDs (FCD:
P = 0.042; HS: P = 0.045), Type of surgery (FCD: P = 0.037; HS: P =
0.015). Remaining factors that may not involve in the outcome are
cataloged in (Table 1)Discussion
Focal lesions of the brain, FCD and HS are the most common
causes for the drug resistant epilepsies [2]. Surgery is generally used to
combat seizures in these cases but post-surgical outcome is not upto
the mark, reasons are unclear, and might be multifactorial [3]. Several
studies have been done to relate clinical factors with the post-surgical
seizure free outcome provided conflicting results due to its less sample
size [13,14,10,16]. The present study involved 576 patients (FCD:
174; HS: 402) who underwent epilepsy surgery. As per our familiarity,
this is the largest case series on focal epilepsies from a single epileptic
centre. Based on our studies more male than female identified for
focal seizures with no difference in ILAE-I and II outcome (FCD: P =
0.382; HS: P = 0.274) conflicting with the previous studies [1]. More
patients were identified with FCD allied focal epilepsies at < 6 years of
age but HS allied epilepsies showed good outcome (FCD: P = 0.702;
HS: P = 0.364) contrasting with earlier studies [18]. Surgery age >18
years have more ILAE-I and II outcome in FCD allied epilepsies (P
= 0.135). Whereas surgery age has no influence on outcome of HS
allied epilepsies (P = 0.151) supported earlier studies [19]. Most of
the HS allied epilepsies had pre-operational auras, but more seizure
free outcome was found in FCD and HS epilepsies with no preoperational
auras (FCD: P = 0.183; HS: P = 0.201), conflicting with
the previous studies [20]. Daily and weekly seizure patients were more
in FCD epilepsies, where as daily, weekly and monthly seizure patients
were more in HS epilepsies. However in both the focal epilepsies, the
seizure free outcome more in the daily and yearly cases (FCD: P =
0.173; HS: P = 0.096) supported by earlier studies [21,22]. Epileptic
patients with focal seizures showed good post-surgical outcome both
in FCD (P = 0.223) and HS (P = 0.196) correlating with the previous
studies [23]. Our study demonstrated TLE associated with HS offered
good post-surgical outcome (P = 0.165) followed by FCD-IIB, IIA,
III, IB and IA (P = 0.087) however, earlier studies have diverse
opinions on histopathology based surgical outcome
[3,24,25,26,27,28,29]. Based on our study, FCD located in temporal lobe and frontal lobe offered good post-surgical outcome, irrespective of the
FCD subtypes (P = 0.123) in correlation with the previous studies
[30,31]. Our study revealed that the above described clinical and
histological factors have no influence on the seizure free outcome
as they are statistically insignificant (P value is > 0.05). Based on the
analysis (univariate), the possible and significant predictive factors
allied with surgery outcome in FCD and HS epilepsies were seizure
durations (FCD: P = 0.053; HS: P = 0.051), IEDs (FCD: P = 0.042; HS:
P = 0.045) and surgical type (FCD: P = 0.037; HS: P = 0.015). Seizure
duration is the time gap between seizure onset and the age of surgery.
Both in FCD and HS, majorly in HS, the seizure duration of < 1 year
exhibited more ILAE-I and II outcome. One conceivable supposition
is that an enduring seizures cause an epileptogenic fuel processes
such as synaptic plasticity, cell proliferation, cell death, inflammation
and immune responses, that finally triggers new epileptic foci,
consequently lower the chance to be seizure free after epilepsy surgery
[14]. IEDs or inter-ictal spikes are bulky flashing electrophysiological
actions found between seizures in epileptic patients. Even though
IEDs happen more regularly than seizures, they are less studied and
the connection to seizures unclear. Generally IEDs happen outside
the brain tissue where the actual site of seizure onset and circulate
toward it, representing that the dissemination of IEDs provides
helpful information to localize EZ [32]. Several exposition studies
depicted that dissecting brain areas of more IEDs improved surgical
upshots in DRE patients [33]. Our studies revealed that patients with
regional and unilateral IEDs got more favorable outcome in case of
HS, whereas in case of FCD, regional IEDs provided good outcome.
Complete resection of epileptic foci (GTR) offered good post-surgical
outcome both in FCD and HS allied epilepsies. Furthermore our
data fairly support the existence of an ongoing epileptogenic process
managed by variety of biochemical and molecular factors, triggered
by frequent seizures, traces of epileptic lesion and IEDs.