Research Article
Imprints of Seizure Rate and Epilepsy Duration on Temporal Lobe Epilepsy Outcome
Pradeep Madhamanchi1,2, Sujatha Peela4, Kishore Madamanchi1, Sita Jayalakshmi3, Manas Panigrahi3, Haritha Ronanki2, Panchareddy Madhava Rao4, SPD Ponamgi5 and Prakash Babu Panithi1*
1Department of Biotechnology & Bioinformatics, University of Hyderabad, Gachibowli, Telangana, India
2Centre for Applied Sciences, Government Degree College (Men)-Srikakulam, Andhra Pradesh, India
3Department of Neurology, Krishna Institute of Medical Sciences, Secunderabad, India
4Department of Biotechnology, Dr. B. R. Ambedkar University-Srikakulam, Andhra Pradesh, India
5Department of Biotechnology, Andra University, Visakhapatnam, India
2Centre for Applied Sciences, Government Degree College (Men)-Srikakulam, Andhra Pradesh, India
3Department of Neurology, Krishna Institute of Medical Sciences, Secunderabad, India
4Department of Biotechnology, Dr. B. R. Ambedkar University-Srikakulam, Andhra Pradesh, India
5Department of Biotechnology, Andra University, Visakhapatnam, India
*Corresponding author: Prakash Babu Panithi, Department of Biotechnology & Bioinformatics, University of Hyderabad, Gachibowli, Telangana, India. E-mail Id: prakash@uohyd.ac.in
Article Information: Submission: 14/08/2023; Accepted: 19/09/2023; Published: 22/09/2023
Copyright: © 2023 Madhamanchi P, et al. This is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
HS associated TLE is the common cause of PRE. Surgery is generally used to control seizures for these patients but most often seizure recurrence observed, reasons are not known. The aim of the study is to evaluate the effects of seizure rate and epilepsy duration on the long term post-surgical outcome
of AEDs and onset age matched 153 HS associated PR-TLE patients. All the patients invariantly associated with HS. Clinical data recorded during 2011 and 2023 obtained from outpatient at the department of Neurology, Krishna Institute of Medical Sciences, Secunderabad, India. EEG, MRI and FluoroJade
stain used to diagnose the TLE-HS in patients. All patients undergone medial temporal lobectomy for HS and assessed for seizure free outcome after first, third and fifth years using Engel’s and ILAE outcome system of classification. Overall 70.8% patients had very good post-surgical outcome (Engel’s-I & II or ILAE-I) in first year, it was reduced to 59.3% in third year and 47.6% in fifth year. The mean seizure rate was 6 per month (range 0.3 – 258 per month). Patients belong to daily and yearly seizure classes had good post-surgical outcome after first year of the surgery (p = 0.43), however mean drop of Engel’s-I or ILAE-I & II outcome after 5th year of the surgery was more in patients with weekly seizures (p = 0.63). Likely the mean epilepsy duration was 13.57
years (range 01 M – 42 years). Patients with less epilepsy duration had good post-surgical outcome than higher duration (p = 0.41). Besides unreliability of Engel’s-I or ILAE-I & II outcome during post-surgical period observed in patients with less epilepsy duration (p = 0.58) and less surgery age (p = 0.32). Through this study we observed that high seizure rate reduced the consistency of the seizure freeness after surgery. On the other side, higher duration of epilepsy and surgery ages lessen the immediate seizure freeness as well as consistency in outcome. However, we did not find any statistical significance (p< 0.05) while analyzing these data. This study suggests the valuation of Histology, Biochemical, and Molecular factors with long-term post-surgical outcome.
Keywords: Seizure Rate; Epilepsy Duration; Hippocampal Sclerosis; Temporal Lobe Epilepsy; Pharmaco Resistant Epilepsy; Engel’s Outcome; ILAE Outcome
Abbreviations
AEDs: Antiepileptic drugs;DN-KIMS: Department of Neurology,
Krishna Institute of Medical Sciences; EEG: Electro Encephalo
Gram;HS: Hippocampal Sclerosis;ILAE: International League Against
Epilepsy; MRI: Magnetic Resonance Imaging;PR-TLE: Pharmaco
resistant temporal lobe epilepsy;TLE: Temporal Lobe Epilepsy.
Introduction
Temporal lobe epilepsy (TLE) is a form of focal epilepsies that is always recalcitrant to antiepileptic drugs (AEDs) known as pharmaco resistant temporal lobe epilepsy (PR-TLE) [1,2]
. Hippocampal sclerosis (HS) is the most common epileptic foci finding in PR-TLE patients where surgery is enormously used to control seizures [3-6]. Despite the seizure freeness allied with epilepsy surgery, sizable number of post-surgical patients remains to have seizures. Also, it has been noticed that decreasing of seizure freeness over the years in patients with seizure free outcome, although AEDs used [7,8] . The motives for surgery failure in PR-TLE patients and lack of seizure free consistency over the post-surgical period are not well acknowledged. One conceivable supposition is that an enduring seizures cause an epileptogenic fuel processes such as synaptic plasticity, cell proliferation, cell death, inflammation and immune responses [7-12], that finally triggers new epileptic foci [13-14]. So it is presumed that higher the seizure rate and longer the epilepsy, the higher the risk of new epileptic foci, consequently lower the chance to be seizure
free after epilepsy surgery. Therefore the seizure rate and duration of epilepsy should be an important prophets of outcome in epilepsy surgery. The purpose of our study was to determine whether there is a
link to seizure rate and duration with long term outcome.
Methods
The study was recorded and conducted as a review at the
Department of Neurology, Krishna Institute of Medical Sciences
(DN-KIMS), Secunderabad, India. Our internal ethical committee
was informed about the study and it has approved. Data from HS
associated PR-TLE patients operated at the DN-KIMS were collected.
Patients were examined and operated on between 2011 and 2023
were reviewed. A total of 153 PR-TLE patients using 3-4 AEDs with
<12 years of onset age were considered for this analysis [Table 1].
Histological studies with fluorojade stain confirmed the association
of HS (Neuronal cell death) in the PR-TLE tissue samples [15].
All patients underwent unvarying presurgical examination like
neuropsychology, EEG and MRI including quantitative hippocampal
volume measurements with T2 relaxation time [16]
and Sodium Amytal (WADA) test [17]. Post-surgical MRI studies in patients
with no significant seizure free showed that the envisioned structures
were resected. Post-surgical upshot data at first, third and fifth year
postoperatively were classified by means of Engel’s classification.
(Engel’s-I = seizure free with rare auras, Engel’s-II = 1 or 2 seizures
per year, Engel’s-III = more than 90% of the seizures reduced, Engel’s-
IV = no significant reduction or worse [18]. Patients falling into the
various subgroups of Engel’s classes were pooled. The International
League against Epilepsy (ILAE) lately advocated a revision of the
classification [19]. In this study Engel’s-I = ILAE 1 and 2, Engel’s-II
= ILAE 3, Engel’s-III = ILAE 4, Engel’s-IV = ILAE 5. The outcome of
the surgery considered into ILAE classification criteria was collected
individually. Student t-test was used to identify the significant
variances.
Result
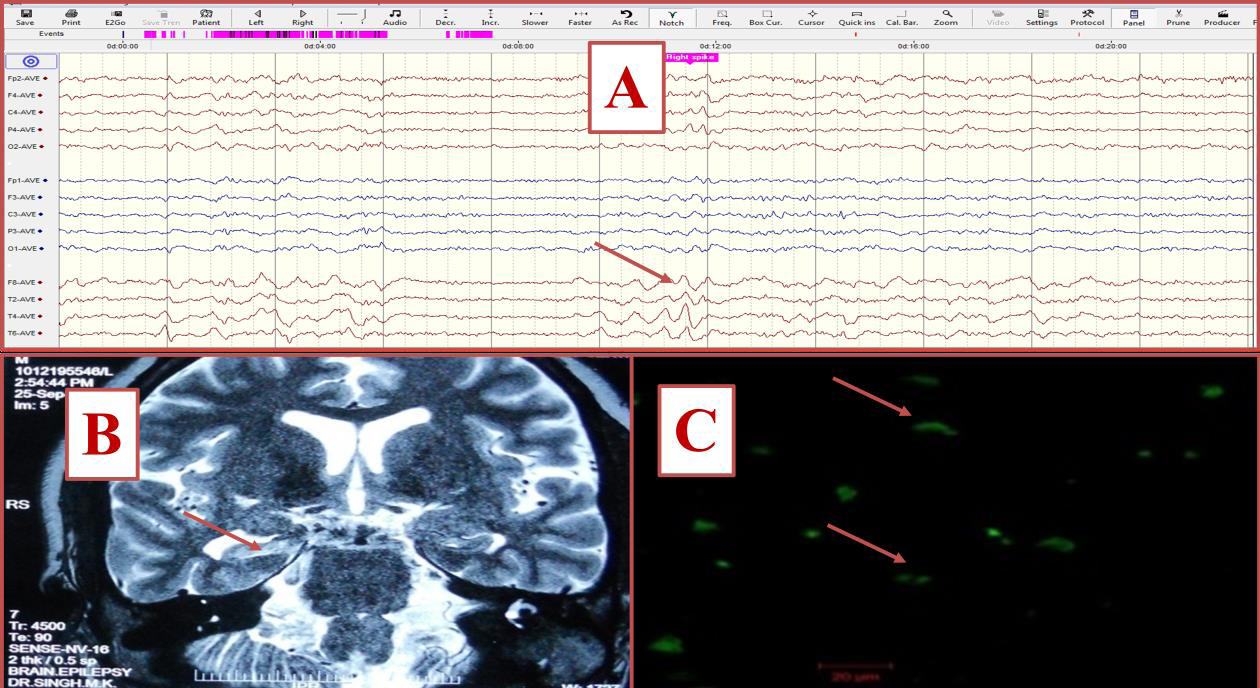
EEG, MRI and histological studies confirmed the association of
HS to PR-TLE patients [Figure 1]. Overall 70.8%, 59.3% and 47.6%
HS allied PR-TLE patients were seizure-free (ILAE-I outcome) in
one year, three years and five years after the surgery. The number of
patients with different outcome classes after 1st, 3rd and 5th years of
surgery were as follows: ILAE-I = 109, 97, 73; ILAE-II = 34, 45, 56;
ILAE-III = 10, 11, 24; ILAE-IV-VI = 00, 00, 00. The mean seizure
rate was 6 per month (range 0.3 – 258 per month). As per the ILAE
outcome chart [19] we noticed that patients be the members of daily
(mean seizures 37.6 per month) and yearly (mean seizures 0.7 per
Figure 1: Electrophysiological and histological examination of HS associated
PR-TLE patients; A. Arrow showing right temporal spikes in EEG recordings;
B. Arrow showing right hippocampal sclerosis in MRI brain image; C. Arrow
showing Confocal image of FluoroJade stained degenerated neurons
(Green color).
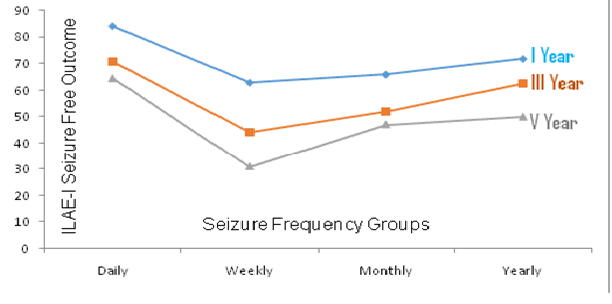
month) seizure classes were good post-surgical outcome after first
year of the surgery (p = 0.61). For instance post-surgical ILAE-I
outcome in different seizure classes: daily = 84%, 70.8%, 64.5%;
weekly = 63%, 44%, 31%; monthly = 66%, 52%, 47%; yearly = 71.8%,
62.5%, 50% after 1st, 3rd and 5th years respectively [Figure 2]. But
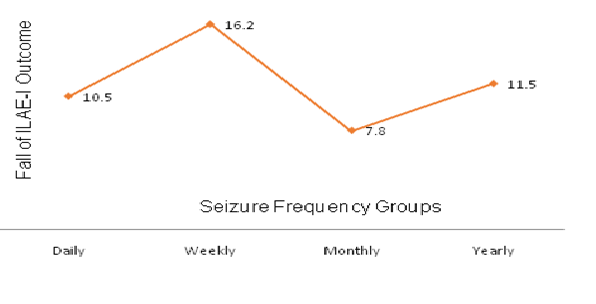
average falling of seizure freeness after 5th year of surgery was more
in patients with weekly seizures (p = 0.63). Mean dropping of ILAE-I
outcome in various seizure classes: Daily = 10.5%, weekly = 16.2%,
monthly = 7.8% and yearly = 11.5% after 5th year of surgery [Figure 3].
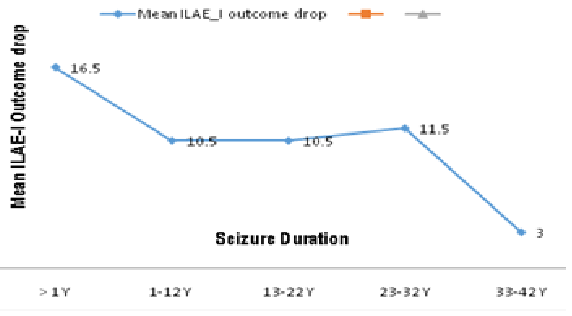
The mean duration of epilepsy was 13.57 years (range 01 M – 42
years). Based on the outcome chart of different epilepsy duration
groups it was observed that patients be the members of less epilepsy
duration groups (<1 year and 1-12 years) were exhibiting good postsurgical
outcome after first year of the surgery (p = 0.41) than more
epilepsy duration groups. For instance post-surgical ILAE-I outcome
in different epilepsy duration groups after 1st, 3rd and 5th years: <1
year = 83%, 67%, 50%; 1-12 years = 92%, 79%, 71%; 13-22 years =
41%, 23.7%, 19%; 23-32 years = 36%, 26%, 13.6%; 33-42 years = 15%,
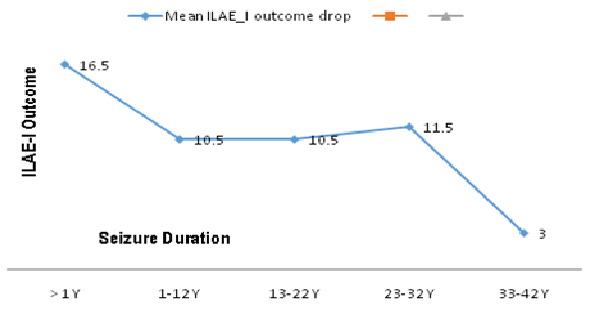
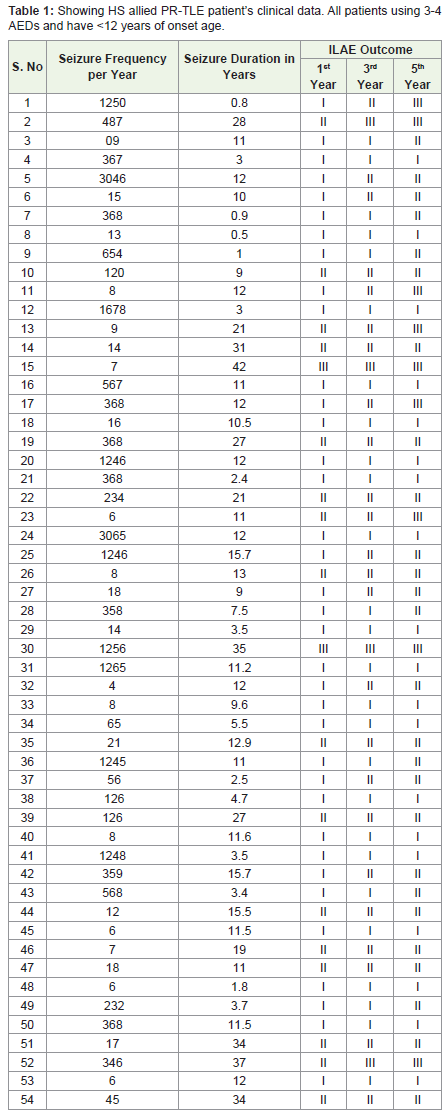
11%, 09% respectively [Figure 4]. Interestingly dipping of seizure
freeness after 5th year of surgery was more in patients with lowest
epilepsy duration. In this study the average falling of ILAE-I outcome
in various epilepsy duration groups: <1 year = 16.5%; 1-12 years =
10.5%; 13-22 years = 10.5%; 23-32 years = 11.5%; 33-42 years = 3%
after 5th year of surgery (p = 0.58) [Figure 5]. Further, we studied the
association of surgery age of patients with different seizure frequency
and epilepsy duration groups. We observed a positive correlation of
surgery age with different epilepsy duration groups and also dropping
of ILAE-I outcome after 5th year of surgery, in illustration the surgery
age of 13.4 years = 8%, 20.4 years = 5.5%, 28.3 years = 7.5%, 38.12 years
= 16.5% and 40.6 years = 18% reduction in seizure free outcome (p =
0.32). The youngest patient was 7 years old at the time of operation
with ILAE-I outcome thereafter the surgery. She had suffered from
epilepsy since the age of 4 years (4 years of epilepsy duration) with
seizure frequency of 8 per year. Similarly the oldest patient was 50
years old at the time of operation with ILAE-III outcome afterwards
the surgery. He had suffered from epilepsy since the age of 24 years
(26 years of epilepsy duration) with seizure frequency of 9 per year.
Figure 2: ILAE-I outcome in various seizure frequency groups after I, III and
V years of surgery. * (Daily: > 365 seizures/year; Weekly: > 56 seizures/year;
Monthly: >12 seizures/year; Yearly: < 12 seizures/year
Figure 3: Mean reduction in ILAE-I outcome in various seizure frequency
groups after V year of surgery. * (Daily: > 365 seizures/year; Weekly: > 56
seizures/year; Monthly: >12 seizures/year; Yearly: < 12 seizures/year
Figure 5: Mean reduction in ILAE-I outcome in various seizure duration
groups after V year of surgery.
Discussion
In this study we observed that, the seizure rate and the duration
that the patients have had HS linked PR-TLE, have a profound effect
on the outcome of their subsequent surgery. We found a trend
for a better outcome in patients with daily and yearly seizures as
well as shorter duration of epilepsy and surgery age which was not
statistically significant. All the PR-TLE patients were homogeneous in terms of onset age, AEDs usage and surgery procedures [1,20-22].
Patient assortment and presurgical investigations were standardized.
The upshot of the surgery considered into ILAE classification criteria
was collected independently and blindly (i.e. with no submission
while collecting the information as to what it was to be analysed for),
to reduce information collection bias. Our study was based on the
results of most other studies, which tried to link up the seizure rate
and duration of epilepsy discretely with post-surgical outcome [23-29]
. Due to polemics in prediction of long term outcome [1,30-32], we used one year, three years and five years next to the surgery for outcome prediction. Our study plainly described that the seizure rate and epilepsy duration govern the seizure predisposition later years
after the surgery. The main advantage of our study was that no patient
was lost throughout the follow-up assessments and all supported well.
Patients who grieved from epilepsy with frequent seizures for a long
time may have greater risk of depressive and cognitive side effects
of epilepsy surgery [33], but some patients can have a tremendous
outcome. This result is imperative when determining whether a patient
should be offered surgery. Furthermore our data fairly support the
existence of an ongoing epileptogenic process, triggered by frequent
seizures and duration of epilepsy within certain surgery age. At least
in our patient population, a kindling process can be entirely included.
Kindling may be related to the seizure rate and duration of epilepsy
besides, lack of statistical significance.