Research Article
Nutrition in Tribal Children of Yercaud Region, Tamil Nadu
Pujitha Sriram Padmanabhan1* and Kanchan Mukherjee2
School of Health System Studies, Tata Institute of Social Sciences, Mumbai, India
Corresponding author: Pujitha Sriram Padmanabhan, School of Health System Studies, Tata Institute of Social Sciences, V.N.Purav Marg, Deonar, Mumbai-400080, Tel: 9820475654: E-mail: pujitha.sriram@gmail.com
Citation: Padmanabhan PS and Mukherjee K. Nutrition in Tribal Children of Yercaud Region, Tamil Nadu. Indian J Nutri. 2016;3(2): 148.
Copyright © 2016 Padmanabhan PS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Nutrition | ISSN: 2395-2326 | Volume: 3, Issue: 2
Submission: 01/11/2016; Accepted: 30/11/2016; Published: 05/12/2016
Abstract
Nutritional status of the child is dependent on several factors. Many tribal communities show high levels of undernutrition. This study was conducted to assess feeding practices of mothers and nutritional status of children in the tribal communities of Yercaud region, Tamil Nadu. This was an observational cross-sectional study. Purposive sampling was done and 110 respondents having children aged 12-23 months were chosen for the study. A semi-structured interview schedule was used for data collection. Data on feeding practices was obtained from mothers. Height and weight of their children was measured.Feeding practices were assessed based on the eight core indicators given by UNICEF in the IYCF policy. Z scores for height for age, weight for age, and weight for height were calculated and compared against WHO standards. Prevalence of timely initiation of breastfeeding, exclusive breastfeeding for 6 months and continued breastfeeding at 12 months was 70, 27.3 and 82.7 percent respectively. Complementary feeding was initiated in the sixth month only in 25.5 per cent of the children. Eighty percent of children achieved dietary diversity whereas only 20 and 17.3 percent of children achieved minimum meal frequency and minimum acceptable diet. Iron supplements were consumed by 24.5 percent of the children. The prevalence of underweight, stunting and wasting in children was 46.4, 71.8 and 23.6 percent respectively. There are gaps between feeding practices advocated in the IYCF policy to what is followed in this tribal community. The prevalence of stunting in children is alarmingly high. There is an urgent need to pay attention to the nutritional status of children in order to avoid deleterious consequences on generations together.
Keywords: Feeding practices; Nutritional status; Children; Tribal communities
Introduction
The World Health Organization (WHO) defines 'Nutrition' asthe intake of food considered in relation to the body's dietary needs.Malnutrition occurs in two forms - Undernutrition (deficiency of essential nutrients in the body) and Overnutrition (excess of nutrients in the body). Infants and young children grow rapidly and require relatively more nutrients (2-3 times) per kg body weight than adults [1]. Undernutrition is an important determinant of childhealth [2]. Stunting or low height for age is an indicator of chronic undernutrition caused by inadequate food intake for longer periods. Wasting or low weight for height indicates acute undernutrition mainly due to frequent diseases and inadequate healthcare facilities. Underweight or low weight for age is an indicator of chronic and acute undernutrition [3]. The most serious forms of under-nutrition are Severe Acute Malnutrition (SAM) and Moderate Acute Malnutrition (MAM), where SAM is defined as a child having a weight-for-height ratio > 3 standard deviations below the mean for their age, and MAM is a height-for-weight ratio > 2 but < 3 standard deviations [4]. Childhood undernutrition alone contributes to over a third of underfive deaths globally [5]. It was estimated in 2007 that 200 million children each year are not developing to their full potential either mentally or physically due to endemic hunger [6].
In developing countries, undernutrition among children is a major public health concern. It is thought to be both a cause and manifestation of poverty. In poorer populations, growth faltering among infants usually occurs shortly after the transition to complementary feeding, because most poor households do not have access to the types of food that can meet the nutritional needs of children [7]. NFHS-3 data (2005-2006) reports that the prevalence of underweight in India increases during the phase from birth to 20-23 months. However, even within India, the percentage of children underweight (55.9), and even with respect to other child health indicators like infant mortality (62.1; NFHS 2005-06), under 5 mortality (95.7; NFHS 2005-06) is higher in Scheduled Tribe (ST) populations than that of the overall population as well as of other disadvantaged socioeconomic groups [8,9].
India has one of the largest tribal populations of the world and tribal communities show greater vulnerabilities to several diseases[10]. The Indian constitution has recognized nearly 700 types of tribal population groups as Schedule Tribes. The total ST population of India stands at 104,281,034 as per 2011 census and accounts for 8.6% of the total population of the country [8]. Tribes have traditionally been socially and economically disadvantaged [11,12]. Tribes show highlevels of undernutrition [13]. Among tribal communities, poverty is as high as 88 percent, underweight about 69 per cent, wasting over 48 percent and stunting over 61 per cent, compared to 69 per cent poverty, 40 per cent underweight, and around 37 per cent of wasting and stunting among non-tribal communities [14]. A study conducted on the Oraon tribes of West Bengal revealed that the nutritional status of children was substantially lower than that of the adult males and females [15]. In another study, it was seen that malnutrition linked disease burden in tribal children of Thane districts, Maharashtra, was as high as 94 percent and 4 percent mortality was attributable to diarrhoea [16]. A study conducted on the Saharia tribes of Rajasthan revealed that prevalence of underweight and stunting among tribal children was significantly higher compared to their rural counterparts [17]. Likewise, Divakar et al. also observed that in Mysore, more tribal children were suffering from Protein-Energy Malnutrition compared to non-tribal children [18].
A child's nutritional foundation is established in the first 36 months of life, where the first 1000 days are considered the most critical [19,20]. Infant and Young Child Feeding (IYCF) practices are a set of recommendations to achieve appropriate feeding of newborn, and children under two years of age in order to achieve optimal nutrition outcomes in populations. IYCF actions are implemented as part of the priority child survival and development programmes of UNICEF and WHO, as well as in the plans of many nations (GOI, 2013). The Lancet series on Maternal and Child Undernutrition-2008, talk of 'Changing Infant and Young Child Feeding (IYCF) behavior' as one of the five major recommended strategies to reduce stunting and child deaths. Early initiation of breastfeeding, exclusive breastfeeding upto 6 months and timely complementary feeding are reported to be very poor in India [20]. While there have been severalstudies conducted to assess the prevalence of feeding practices of mothers, most of them have concentrated on breastfeeding practices alone. Nutritional problems of various tribal communities located at various stages of development are full of obscurities and very little scientific information on their dietary habits and nutritional status are available due to lack of systematic and comprehensive research investigations [8]. Tamil Nadu is one of India's more progressive states, ranking in top 3 on several economic and social indicators. However, the UNICEF reports that within Tamil Nadu, several regional and social disparities exist, in addition to several caste and gender-related poverty issues posing a great problem for children belonging to some regions, especially those from socially excluded communities such as Scheduled Castes and Scheduled Tribes. Scheduled Tribe population in Salem district is estimated to be roughly 3.43% of the total population in Tamil Nadu, and the number of tribals in Yercaud block of Salem district are reported to be 28,118 [21]. While there have been several studies done on the tribals living in the Nilgiris in Tamil Nadu, there have been very limited studies on the developmental status of the other tribal groups there [22]. This study was conducted with an aim to understand the feeding practices of mothers and nutritional status of children in the tribal communities of Yercaud region, Tamil Nadu.
Materials and Methods
Operational definitions
The feeding practices of mothers were analysed based on the eight core indicators given by UNICEF (2012) namely - Early initiation of breastfeeding, Exclusive breastfeeding for 6 months, Continued breastfeeding at 1 year, Introduction of solid, semi-solid or soft foods, Minimum dietary diversity (MDD), Minimum meal frequency (MMF), Minimum acceptable diet (MAD), Consumption of ironrich or iron-fortified foods [23]. Nutritional status of the children was assessed based on the WHO Z scores for height-for-age, weightfor- age and weight-for-height where Z scores less than -2 standard deviations from the mean were considered stunting, underweight and wasting respectively.
Study area
Yercaud in Salem district, Tamil Nadu, is very famous as a hillstation. Yercaud is located in the Shevaroys range of hills in the Eastern Ghats, at an altitude of 1515 metres. Majority of the population in Yercaud are tribals, and the indigenous inhabitants of Yercaud areknown as 'Malaialis' (Hill men) or Vellalas. Respondents for this study were chosen from Manjakuttai, Nagalur, Semmanatham, Thalaisolai, Velur, Vellaikadai and Vazhavanthi which are all villages in the Yercaud block.
Research design
Keeping in mind the objectives of the study, a quantitative approach was applied to the methodology. This was an observational cross-sectional study. Data on feeding practices were to be collected from the mothers of children aged 12-23 months of age. This agegroup of children twelve months of age onwards was considered because the likelihood of the child having been introduced to all the food groups is more than at six months of age onwards. Purposive sampling method was used throughout the study. Data was collected from 110 mother-child pairs. The decided number of respondents from each of these areas were identified with the help of keyinformants, and mothers were chosen on the basis of inclusion and exclusion criteria. Mothers with children in the age-group of 12-23 months were recruited for data on feeding practices, and children aged 12-23 months were chosen for assessment of their nutritional status. Both the mother and child needed to be present at the time of data collection. Children with medical complications or physical disabilities that can affect dietary intake, respondents not residing in that area/not belonging to the tribal community and respondents who were unwilling to participate in the study were excluded from the study.
Data collection and anthropometric measurements
Permission was obtained from the office of the Deputy Director of Health Services, Salem district, and the respective Block Medical Officers (BMO) of the Yercaud block area to conduct the study. Data collection was then done by first establishing contact with a Sector Health Nurse (SHN) in Yercaud block, who helped identify the villages. The respondents in these villages were then identified with the help of the Accredited Social Health Activists (ASHAs) and Village Health Nurses (VHNs) there. Once the respondents were identified and chosen by means of the inclusion and exclusion criteria, their consent was taken before proceeding with the interview. A one-on-one interview was conducted with each of the respondents with the help of a semi-structured interview schedule, and data on the socio-demographic profile, medical history of the mothers and feeding practices was obtained, following which anthropometric measurements of the child were taken to calculate Z scores and assess the nutritional status. Weight values for the child were obtained using calibrated spring scales. A non-stretchable tape was used to measure the height of the children, where the children were made to stand erect, with the heels, buttocks, shoulders and the head touching the wall, and the value was recorded to the nearest cm. Data collection was done over a duration of three months, from July 2015 to September2015. The objectives of the study were explained to the respondents and they were encouraged to ask the researcher for any clarifications. They were assured by the researcher that their privacy would be respected and confidentiality would be maintained. Participants were allowed to withdraw from the study at any stage.
Analysis
All the data was recorded in the software Statistical Package forSocial Sciences (SPSS) Version 20. Z scores for nutritional status werecalculated by use of software WHO Anthro Version 3.2.2. To describe about the data, descriptive statistics mainly frequency analysis, percentage analysis, mean and S.D were used.
Results
Socio-demographic data
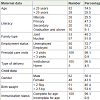
Data for this study was collected from 110 mother-child pairs.Table 1 gives the socio-demographic profile of the respondents who participated in the study.
Maximum proportion (74.5%) of the women belonged to the age-group of below or equal to 25 years. About half of the mothers (47.3%) who participated in the study had completed education up to the primary school level, followed by 25.5 per cent mothers who were illiterate. Fifty seven per cent of the women belonged to nuclear families, and a majority (80%) of them had been unemployed in the last twelve months. Almost all of the mothers (99.1%) reported that they had more than three prenatal care visits to a healthcare facility during the course of their pregnancy, and 95.5 per cent of them reported to have had institutional deliveries.
The mean age of the children was 18.13 ± 3.82 months. Around fifty six per cent of the children were males. Only around fifty four per cent of the children were born with normal birth weight, i.e. greater than 2.5 kg. However, most children (99.1%) were fully immunized for age.
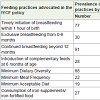
Feeding practices
Table 2 demonstrates the prevalence of the various feeding practices in the community. It is seen that the prevalence of timely initiation of breastfeeding was seventy per cent. Exclusive breastfeeding from 0-6 months was followed by only around twenty seven per cent of the mothers. Continued breastfeeding beyond 12 months of the child's age was reported by 82.7 per cent of the mothers. Complementary feeding was initiated at completion of the sixth month only in 25.5 per cent of the children. Eighty percent of children achieved minimum dietary diversity (MDD) whereas only 20 and 17.3 percent of children achieved minimum meal frequency (MMF) and minimum acceptable diet (MAD) respectively. Iron supplements were consumed by 24.5 percent of the children.
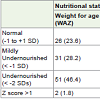
Nutritional status of children
Table 3 gives details about the nutritional status of children in Yercaud tribal region. The table shows that around twenty four per cent children had normal weight for age (WAZ). Around forty six per cent children had WAZ scores less than -2 SDs, indicating underweight. Only 8.2 per cent of the children had normal height for age (H/A) Z scores. Stunting i.e. HAZ scores less than -2 SDs, was seen in 71.8 per cent of children. Close to thirty seven per cent of the children had normal weight for height (WHZ). Around twenty four per cent of the children showed wasting with WHZ scores less than -2 SDs.
Discussion
One of the objectives of this study was to identify the gaps that exist in the feeding practices followed by mothers in the communityto what is advocated in the IYCF policy given by UNICEF. The IYCF policy issues guidelines both with respect to breastfeeding and complementary feeding practices. It advocates that breastfeeding needs to be initiated as early as possible, avoiding delay beyond an hour, for all normal newborns (even for those born by Cesarean section). In this study, it was observed that seventy per cent mothers had initiated breastfeeding within an hour of the child's birth. The main reason given for delay in initiation of breastfeeding was Caesarean deliveries, followed by other reasons like no milk production, baby not latching on to the breast or unable to suck. With respect to exclusive breastfeeding, The IYCF guidelines recommend that it needs to be strictly followed from 0-5 months of the child's life, and that no other fluids or food should be given to the child unless medically indicated. In this study, the prevalence of exclusive breastfeeding from 0-5 months was dismally low (27.3%) and this is mainly attributed to the practice of prelacteal feeding. The most common prelacteal feeds reported to having been given were sugar water and honey. Swain (1985) also found that among the Santaltribe in northern Orissa, immediately after the child's birth, honey orjaggery was given to the child as they believed that these substancescould help the child resist hunger [24]. In this study, prelacteal feeding was prevalent for several reasons mainly pertaining to family customs and tradition, problems with establishing lactation and so on. Insufficient milk supply, problems with lactation and importance of solid food for the growing baby were some of the other reasons given by the mothers for not following exclusive breastfeeding.Another study also reported that insufficient milk supply was one of the most common reasons given by mothers for not continuing to breastfeed [25]. One of the other optimal breastfeeding indicatorsis continued breastfeeding beyond twelve months of age where it is advocated that even with introduction of optimal complementary feeding, breastfeeding should be continued for at least two years and beyond, depending on the choice of both the mother and child. The IYCF guidelines suggest that even after twelve months of age, the frequency of breastfeeding, including night feeds, should be 4-6 times in twenty four hours. The mothers in this tribal area showed high prevalence of continued breastfeeding beyond twelve months (82.7%). Another study reported that continued breastfeeding rate of the child at one year of age was 99.7 per cent and 87.2 per cent at two years of age [26].
In order to ensure that a growing infant is able to meet his/ her nutritional requirements, the IYCF policy recommends that complementary feeds needs to be introduced to the child at six completed months of age. The guidelines further state that the feeds need to be appropriately thick and of homogenous consistency. In this study, all the 110 children (100%) had been started on complementary feeds, however, only 25.5 per cent of the children had been introduced to complementary feeds at six months of age. A study conducted in West Bengal showed that 55.8 per cent of mothers initiated complementary feeding during the 6th-8th month [27].
As a measure to improve the quality of complementary feeds, the WHO-UNICEF Global Strategy for Infant and Young Child Feeding (GSIYCF) identified seven food groups based on research that showed the critical importance of each in the complementary feeding diet (UNICEF, 2012). It is recommended that a child aged 6-23 months receives complementary feeds from a minimum of four groups or more. If the child receives this, he/she is said to have achieved minimum dietary diversity. In this study, eighty per cent of the children had achieved MDD. Most commonly consumed food groups were cereals and pulses. The use of different types of millets like foxtail millet, little millets as part of traditional diets were also noted. Fruits were the most infrequently provided to the children, mainly because the different kinds of fruits growing there in those hilly regions were sold off in the markets in the plains and weren't kept for consumption by families. In another study conducted, itwas observed that the proportion of infants aged 6-8 months who consumed eggs (7.5%), fruits and vegetables other than those rich in vitamin A (29.6%) and flesh foods (35.2%) was low, and in the children aged 6-23 months, the MDD was seventy one per cent, which is considerably lower than what was observed in this study [28]. Thehigher prevalence of MDD in this study could be because children from twelve months of age onwards were only included in the study, by which time they would developmentally be ready to include foods of a lot more variety and food groups than at six months of age.
The IYCF policy also issues guidelines with respect to the minimum number of times the child needs to be fed semi-solid/ solid food in a day, called the Minimum Meal Frequency (MMF). It is recommended that children who are continued to be breastfed be given a minimum of 3-4 complementary feeds a day, with 1-2 snacks in between. Children who are not breastfed are expected to be given five complementary feeds a day, with 1-2 snacks in between. In this study, only twenty percent of the children were reported to being fed at least the minimum number of times required for a child of that age. This probably could be linked to the very high prevalence of continued breastfeeding beyond one year of child's age in these tribal communities, where the mothers may possibly be substituting complementary feeds with breastfeeding. Few studies have reported a far greater proportion of children aged 6-23 months having achieved MMF (41.5% and 88% respectively) [28,29]. One possible explanation for this could be that they included children from six months of age onwards where the number of times complementary feeds to be given are lesser than at twelve months of age onwards.
The effectiveness of complementary feeds meeting both the macronutrient and micronutrient requirements of the child depend equally on the quality and the quantity of the complementary feeds. When a child has achieved both the MDD and MMF, it is said that the child has achieved the Minimum Acceptable Diet (MAD) that a child of his/her age is expected to receive. In a secondary data analysis of the NFHS-3 data [29], it was found that only 9.2 per cent of the children met the MAD requirement, while in this study it was slightly higher (14.15%).
The ICMR Recommended Dietary Allowances of iron for a child who is 12-23 months is 9 mg/day [19]. It is expected that this requirement of iron is met by the diet the child is consuming, or byconsumption of suitable iron supplements/ iron-fortified food. In thisstudy, it was observed that the overall prevalence of consumption ofiron supplements by children was 17.16 per cent. Even those childrenwho were consuming iron supplements were prescribed those by their physicians due to recurrent infections and illnesses.
The other objective of this study was to assess the nutritional status of the children living in this region. It was seen in this study that several children showed different forms of undernutrition, stunting being the most prevalent. Stunting is an indicator of chronic undernutrition, and these alarmingly high levels of stunting in the children here hint at nutritional deprivation even in their infancy stage. Almost half the children in this study (46%) were even born with low birth weights, and this could probably be attributed to nutritional inadequacy right from fetal life. In tribal populations, maternal malnutrition is a serious health problem, especially in those women who have had closely spaced multiple pregnancies [8]. Thus, remedial measures for stunting cannot target children alone without concentrating on the health and nutritional status of the adolescent girls and mothers in the population. In a study on the Gond tribes of Madhya Pradesh [30], there was a prevalence of sixty per cent underweight in the children there, while in this study, the proportion of children who were underweight was slightly lesser (46.4%). A study conducted on the children of the Kamar tribes of Chhattisgarh, India also documents high levels of undernutrition in all three forms (underweight, stunting and wasting) in both boys and girls [31]. Another study conducted on children belonging to the Lodha tribes of West Bengal also reports a high prevalence of severe undernutrition [32].
Conclusion
This study brought to light that there are several gaps that exist between what is advocated in the policy to what is followed by the mothers in these tribal communities. These gaps that exist between feeding practices advocated in the IYCF policy and what is followed in the community need to be addressed soon in order to improve the nutritional status of the children in the country. Mothers need to be educated appropriately regarding feeding practices and the need to follow proper hygiene and sanitation practices. The alarming levels ofundernutrition (especially stunting) in the tribal children of Yercaud region requires immediate attention in order to avoid perpetuating effects of undernutrition on generations together. Special attention needs to be given to these indigenous/tribal populations, with more inclusive policies and action, because these people are often cutoff from mainstream society, and may not be aware and hence not benefit from the several schemes that are provided. Also, if there are disparities based on caste, they need to be addressed soon, so that this segment of the population also shows improvements in health and developmental status.
This study has a few limitations. The participants for this study were selected by means of purposive/judgment sampling based on the information given by the key-informants, and so generalizability of the results may be limited. As data collection was done in places like sub-health centres or Anganwadi centres where all these mothers were aggregated together, there may have been misreporting due to perceived lack of privacy or instances where some of the responses given may have been biased by the responses given by others. Further qualitative or exploratory studies can be conducted to obtain deeper insights on feeding practices.
Nevertheless, this study has shown the feeding practices followed by mothers in this tribal community and the extent of undernutrition in the children here, on which there are no other published articles, to the best of our knowledge. Following are a few recommendations based on the results of this study.
• Have specialized lactation counsellors or training for the stafffrom the healthcare system to deal with the lactation issues of the women.
• Employ healthcare staff from within the community itself as they would have a keener sense of the logistics and the intricate details required to build sufficient rapport with the community.
• Research on the nutrient value of locally consumed foods, so that accordingly the capacity of family and local groups to prepare age-appropriate complementary food for children with these locally consumed ingredients could be strengthened.
• Some exploratory qualitative studies could be done to better understand the attitudes, beliefs and values influencing feeding behaviour .
• Frequent screening and monitoring of children upto 36 months of age needs to be done before irreversible changes take place affecting growth and development.
References
- Gopalan C, Sastri BV, Balasubramanian SC (1989) Recommended dietary allowances for Indians. Nutritive Value of Indian Foods 92.
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371: 243-260.
- Martorell R, Ho TJ (1984) Malnutrition, morbidity, and mortality. Popul Dev Rev 10: 49-68.
- WHO (2009) WHO child growth standards and the identification of severe acute malnutrition in infants and children: a joint statement by the World Health Organization and the United Nations Children's Fund. World Health Organization, Geneva.
- UNICEF (2012) The state of the world's children 2012: children in an urban world.
- Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, et al. (2007) Developmental potential in the first 5 years for children in developing countries. Lancet 369: 60-70.
- Scott J, Campbell D, Davies M (2008) Mothers and infants: Public Health Nutrition: From principles to practice. Allen & Unwin, Australia.
- Kshatriya GK (2014) Changing perspectives of tribal health in the context of increasing lifestyle diseases in India. J Environ Soc Sci 1: 1-7.
- (2007) National Family Health Survey (NFHS-3) 2005- 2006. Ministry of Health and Family Welfare.
- 10.Shrivastava SR, Shrivastava PS, Ramasamy J (2013) Implementation of public health practices in tribal populations of India: challenges and remedies. Healthcare in Low-resource Settings 1: 3.
- Singh AK, Rajyalakshmi C (1993) Status of tribal women in India. Soc Change 23: 3-18.
- Basu SK (1993) Health status of tribal women in India. Soc Change 23: 19-39.
- Bawdekar M, Ladusingh L (2008) Contextual correlates of child malnutrition in rural Maharashtra. J Biosoc Sci 40: 771-786.
- Tagade N (2012) Food insecurity in tribal regions of Maharashtra: explaining differentials between the tribal and non-tribal communities. The Institute for Social and Economic Change.
- Mittal PC, Srivastava S (2006) Diet, nutritional status and food related traditions of Oraon tribes of New Mal (West Bengal), India. Rural Remote Health 6: 385.
- Tekale NS (2006) Health and nutrition status of Warli tribal children in Thane district of Maharastra. In: Proceeding of National Symposium on Tribal Health, pp. 221-223.
- Rao KM, Kumar RH, Venkaiah K, Brahmam GN (2006) Nutritional status of Saharia - A primitive tribe of Rajasthan. J Hum Ecol 19: 117-123.
- Divakar SV, Balaji PA, Poornima S, Varne SR, Ali SS, et al. (2013) A comparative assessment of nutritional and health status between tribal and nontribal under five children of Mysore, India. Muller J Med Sci Res 4: 82.
- Ministry of Health and Family Welfare (2013) Guidelines for enhancing optimal Infant and Young Child Feeding Practices, New Delhi.
- Menon P, Bamezai A, Subandoro A, Ayoya MA, Aguayo V (2015) Age-appropriate infant and young child feeding practices are associated with child nutrition in India: insights from nationally representative data. Matern Child Nutr 11: 73-87.
- Planning Commission. Government of India. Census of India 2011.
- Mann RS (1996) Tribal Scenario and developmental Planning in Tamil Nadu. In: Sudarsan V, Xavier R (Eds). Tribes of India: Ongoing challenges, MD Publications Pvt. Ltd.
- World Health Organization (2009) Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals.
- Swain L (1985) Santal tribes: Infant feeding practices. Social Welfare 3: 22-23.
- Hector D, King L, Webb K, Heywood P (2005) Factors affecting breastfeeding practices. Applying a conceptual framework. New South Wales public health bulletin 16: 52-55.
- Banapurmath CR, Nagaraj MC, Banapurmath S, Kesaree N (1996) Breastfeeding practices in villages of central Karnataka. Indian Pediatr 33: 477-479.
- Sinhababu A, Mukhopadhyay DK, Panja TK, Saren AB, Mandal NK, et al. (2010) Infant-and young child-feeding practices in Bankura district, West Bengal, India. J Health Popul Nutr 28:294-299.
- Senarath U, Godakandage SS, Jayawickrama H, Siriwardena I, Dibley MJ (2012) Determinants of inappropriate complementary feeding practices in young children in Sri Lanka: secondary data analysis of Demographic and Health Survey 2006-2007. Matern Child Nutr Suppl 1: 60-77.
- Patel A, Pusdekar Y, Badhoniya N, Borkar J, Agho KE, et al. (2012) Determinants of inappropriate complementary feeding practices in young children in India: secondary analysis of National Family Health Survey 2005-2006. Matern Child Nutr Suppl 1: 28-44.
- Rao VG, Yadav R, Dolla CK, Kumar S, Bhondeley MK, et al. (2005) Undernutrition & childhood morbidities among tribal preschool children. Indian J Med Res 122: 43-47.
- Mitra M, Kumar PV, Chakrabarty S, Bharati P (2007) Nutritional status of Kamar tribal children in Chhattisgarh. Indian J Pediatr 74: 381-384.
- Bisai S, Bose K, Ghosh A (2008) Nutritional status of Lodha children in a village of Paschim Medinipur district, West Bengal. Indian J Public Health 52: 203-206.