Case Report
Complex Congenital Cardiac Anomalies and Complex Tapvc-A Case Report
Vasudha N1*, Pramod N2 and Jeetendra P3
1Department of Anatomy, University Kasaba Bawada, India
2Department of Radiodiagnosis, D.Y.Patil Medical College, India
3Department of Radiodiagnosis, D.Y. Patil Medical College, India
*Corresponding author: Vasudha N, Professor Department of Anatomy, D. Y. Patil Medical College, DY Patil Education Society; Deemed to be University Kasaba Bawada, Kolhapur, Tel: 9665730990; E-mail: dr.vasudhanikam@gmail.com
Copyright: © 2019 Vasudha N, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Information: Submission: 07/05/2019; Accepted: 19/09/2019; Published: 23/09/2019
Abstract
Complex cardiac anomalies are the main cause of infant mortality. Early diagnosis and proper mode of treatment is essential in these cases. Screening of
the patients detects the significant congenital heart defects. We present a case of complex cardiac anomalies with Atrial Septal Defect (ASD), Total Anomalous
Pulmonary Venous Connection (TAPVC), dilated right atrial and right ventricular chambers, Patent Ductus Arteriosus (PDA), Persistent Left Sided Superior
Vena Cava (PLSVC).
Keywords
Total anomalous pulmonary venous return; Diagnostic imaging; Congenital heart defects; Echocardiography, Patent ductus arteriosus; Persistent left superior vena cava
Introduction
Congenital heart disease affects almost 1 in 100 newborn babies
worldwide [1]. Congenital heart defects remain the most common
congenital anomalies in live births and are the main cause of infant
mortality in the developed world. Congenital heart disease is defect
in heart and major blood vessels including structural, chromosomal,
genetic, biomechanical defects and malformations [2]. Patients
with CHD frequently suffer from broad spectrum of subsequent
neurological deficits, including motor, cognitive, behavioural,
social and attention abnormalities [3]. Congenital cardiovascular
malformations present some of the most interesting and difficult
challenges in medicine and the repair of heart defects requires
advanced technological interventions and they are among the most
costly defects to manage [4].
Congenital heart defects are anatomically, clinically, epidemiological and developmentally heterogenous. There are eight major malformations, and these are
1. Conotruncal
2. Atrioventricular Septal Defect (AVSD)
3. Total Anomalous Pulmonary Venous Return (TAPVR)
4. Left Ventricular Outflow Tract Obstruction (LVOTO)
5. Right Ventricular Outflow Tract Obstruction (RVOTO)
6. Septal
7. Heterotaxy
8. Complex [5].
Here we report a case of 6 months old baby girl with complex
cardia anomalies.
Case Report
A 6 months old baby girl was referred for screening by
paediatrician. On examination, the patient had dyspnoea, fever, and
mild cyanosis. There was history of recurrent chest infection, low
oxygen saturation and frequently required oxygen supplementation.
On auscultation, there was continuous machinery murmur. The
patient was advised for X-ray chest, 2D echocardiography and CT
pulmonary angiography.
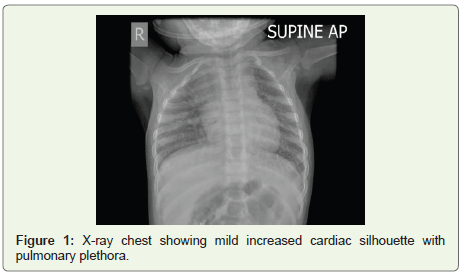
X-ray chest revealed pulmonary plethora. There was enlargement
of blood vessels in both the lungs. There was right upper lobe
consolidation and mild pneumonia was present. There was mild
cardiomegaly that was suggestive of septal defect (Figure 1). 2D
echocardiography revealed large ASD with abnormal pulmonary
venous draining and PDA. There was dilatation of right atrial and
right ventricular chambers with severe tricuspid regurgitation due to
right heart volume overload.
CT Pulmonary angiography revealed following findings;
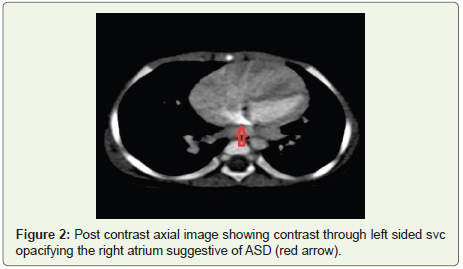
1. Large ASD- (Figure 2).
2. Dilated RA and RV.
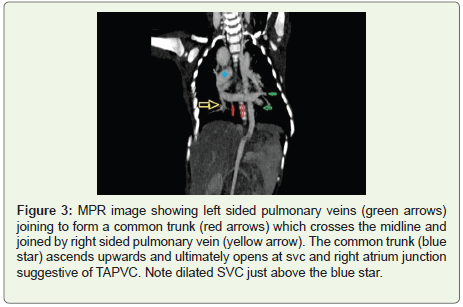
3. Supracardiac type TAPVC (Figure 3).
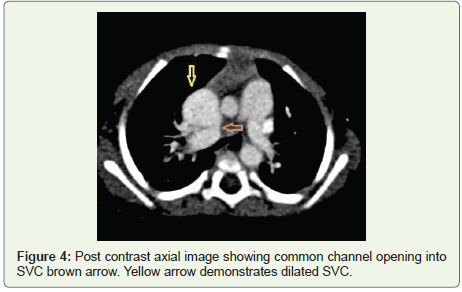
4. Dilated SVC (Figure 4).
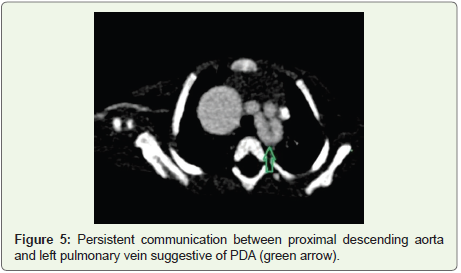
5. PDA (Figure 5).
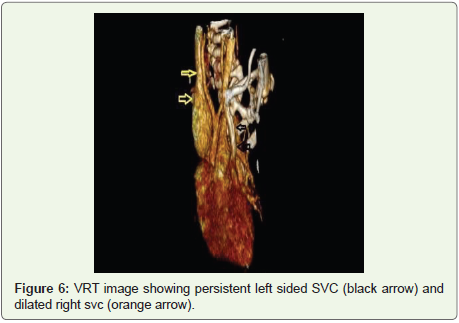
6. Left sided persistent superior vena cava draining into coronary sinus (Figure 6)
All these findings are suggestive of complex TAPVC with multiple
cardiac anomalies.
Discussion
Patients with CHD frequently suffer from a broad spectrum
of neurological deficits including motor, cognitive, behavioural,
social and attention abnormalities [3]. In our case, the baby inspite
of suffering from such complex cardiac anomalies there was no
neurological deficits seen.
The cardiac pathology in patients with TAPVC shows interatrial
septal defects, cardiomegaly, prominent pulmonary trunk, increased
pulmonary vascularity on x-ray, low oxygen saturation ranging from
80% to 90% on oximeter. There is right atrial enlargement with right
ventricular hypertrophy [6]. Clinically patients with TAPVC may
have congestive cardiac failure or profound cyanosis due to interatrial
communication and patency of pulmonary venous flow [7]. However,
in our case, complex cardiac anomalies were present; there was RA
and RV dilatation, low oxygen saturation and mild cyanosis was
present. There were no signs of congestive cardiac failure.
TAPVC is not a problem during fetal development due to high
pulmonary vascular resistance and shunting blood flow through
foramen ovale. However, the heart of patient with TAPVC has
no direct pulmonary connection to the left atrium; thus, severe
pulmonary congestion and pulmonary hypertension can occur after
closing the ductus arteriosus [8]. However, in our case pulmonary
hypertension was not revealed as the patient had PDA.
Figure 2: Post contrast axial image showing contrast through left sided svc opacifying the right atrium suggestive of ASD (red arrow).
Figure 3: MPR image showing left sided pulmonary veins (green arrows) joining to form a common trunk (red arrows) which crosses the midline and joined by right sided pulmonary vein (yellow arrow). The common trunk (blue star) ascends upwards and ultimately opens at svc and right atrium junction suggestive of TAPVC. Note dilated SVC just above the blue star.
Figure 4: Post contrast axial image showing common channel opening into SVC brown arrow. Yellow arrow demonstrates dilated SVC.
Figure 5: Persistent communication between proximal descending aorta and left pulmonary vein suggestive of PDA (green arrow).
Figure 6: VRT image showing persistent left sided SVC (black arrow) and dilated right svc (orange arrow).
Four types of TAPVC are classified based on the location of
pulmonary venous drainage these are:
a) Supracardiac
b) Cardiac
c) Infracardiac
d) Mixed
a) Supracardiac (Type-I TAPVC) is most common, accounting
for approximately 44% of cases. In this type, drainage most commonly
occurs via a vertical vein to the left brachiocephalic vein. Rarely,
supracardiac TAPVC may drain directly to the right SVC, left SVC
or azygous system.
Most commonly in supracardiac type the pulmonary veins drain
to a confluence posterior to the left atrium. An ascending vertical
vein originates from this confluence and travels behind the left atrial
appendage and usually, anterior to the left pulmonary artery. However
occasionally this vein may travel posterior to the left pulmonary
artery and may become trapped in a “vice” between the dilated artery
and left bronchus, leading to pulmonary venous obstruction…the
vertical vein finally drains into the innominate vein. Occasionally the
site of entrance to the innominate vein may also be narrowed, leading
to obstruction. The innominate vein and SVC are dilated. The right
heart is usually dilated due to the volume overload.
b) Cardiac (Type-II TAPVC) which represents approximately
21% of TAPVC cases, pulmonary veins drains either to the coronary
sinus or directly into the right atrium. the pulmonary veins and
coronary sinus are significantly dilated and echocardiography shows
a characteristic “whale” tail appearance. Obstruction is unusual in
this form of TAPVR.
c) Infracardiac (Type-III TAPVC) represents approximately 26%
of cases of TAPVC and drains below the diaphragm to a systemic
vein- the IVC, a hepatic vein, or the azygous system, or the portal
venous system. The draining pulmonary veins in this type of TAPVC
may be obstructed, frequently at the level of diaphragm, because of
extrinsic narrowing, resulting in pulmonary edema with a normal
size cardiac silhouette on chest radiography. In the infra cardiac type
of TAPVR, the pulmonary venous confluence is usually posterior
to the left atrium and vertically oriented. From here, a descending
vein arises and passes through the oesophageal hiatus. Although
pulmonary venous obstruction may occur in any type of TAPVC, it
is most common in the infra cardiac form being represented in upto
78% of patients.
d) Mixed (Type-IV TAPVC) the final type of TAPVC is diagnosed
when the location of pulmonary vein drainage is mixed. In this form
pulmonary veins drain to at least two different locations, including a
brachiocephalic vein, SVC, azygous vein, coronary sinus, right atrium
or below the diaphragm. This type of pulmonary venous drainage
accounts for approximately 9% of TAPVC cases. An example includes
connection of the right pulmonary veins to the coronary sinus and
connection of the left pulmonary veins to the innominate vein [7,9]
Although obstruction can occur in any type of TAPVC, it is
most commonly encountered in the infra cardiac type. There are
various complications of obstructed TAPVC leading to hypoxemia,
pulmonary hypertension and pulmonary vascular obstructive disease
[8,10]. However, our case represents supracardiac type of TAPVC
with low O2 saturation, mild cyanosis but no signs of pulmonary
hypertension as the patient had PDA
Embryologically TAPVC results from early atresia or failure of
common pulmonary veins to develop, with persistence of at least one
connection to the cardinal or the umbilical vitelline venous system.
TAPVC is a cause of neonatal cyanosis and can result in rapid death
when blood is not shunted from right side of heart to the left side.
Isolated TAPVC is diagnosed if the patient has ASD, PDA or both.
Complex TAPVC is diagnosed if the patient has other intracardiac
lesions in addition to ASD or PDA [10].
Our case represents complex TAPVC supracardiac type as along
with ASD, PDA other associated anomalies, which were seen are
persistent left sided superior vena cava draining in dilated coronary
sinus.
Persistent left sided superior vena cava is one of the most frequent
anomalies of systemic venous circulation in 0.3-0.5% of general
population and in 4.3% of those with CHD. In most patients with
persistent left superior vena cava, a right superior vena cava is also
present, and both normally drain into right atrium through dilated
coronary sinus [11,12]. In our case there was persistent left superior
vena cava draining into dilated coronary sinus as well as dilated right
superior vena cava was present.
Thus, in the patients with CHD and complex TAPVC correct
delineation of anatomy and associated cardiovascular anomalies is
crucial while planning the treatment. Hence, the baby was referred to
cardiologist for further management and treatment.
Conclusion
With improvement in imaging techniques, it is possible
to make accurate diagnosis of complex cardiac anomalies. 2D
echocardiography and CT pulmonary angiography imaging is
effective in the diagnosis of complex TAPVC. This case study is a
contribution to the knowledge of complex cardiac anomalies.
Acknowledgement
Eureka Diagnostic Centre; Kolhapur and DY Patil Education
Society supported this work; Deemed to be University; D.Y. Patil
Medical College; Kolhapur. Thanks to Chancellor, Vice Chancellor,
Pro Vice Chancellor, Registrar and Dean of DY Patil Education
Society’s Deemed to be University and D.Y. Patil Medical College,
Kolhapur. Thanks to Dr. Pramod Nagure, Dr Jeetendra Patil and my
colleagues of Department of Anatomy for their support.