Case Report
Imaging Features of Pancreaticopleural Fistula - A Frequently Missed Complication of Chronic Pancreatitis
Vijayendra A* and Biswadeep R
Department of Radiodiagnosis, All India Institute of Medical sciences, India
Corresponding author: Vijayendra A, Department of Radiodiagnosis, All India Institute of Medical sciences, Bhubaneshwar, Orissa, India, Tel no: +91- 9747178161; E-mail: drvijayendra11@gmail.com
Citation: Vijayendra A, Biswadeep R. Imaging Features of Pancreaticopleural Fistula - A Frequently Missed Complication of Chronic Pancreatitis. Indian J Appl Radiol. 2018;4(1): 129.
Copyright ©2018 Vijayendra A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Applied Radiology | Volume: 4, Issue: 1
Submission: 20/09/2018; Accepted: 07/11/2018; Published: 12/11/2018
Abstract
Pancreaticopleural Fistula (PPF) is one of the rare complications of acute and chronic pancreatitis, more commonly chronic pancreatitis. It is characterized by the presence of high amylase and lipase levels in pleural fluid resulting from abnormal communication between the pancreatic duct and/or pancreatic pseudocyst and the pleural cavity [1,2]. It usually presents as massive left sided hemorrhagic pleural effusion. To our knowledge, very few cases have been reported on pancreticopleural fistulas as it is a rare complication. Diagnosing this rare entity is extremely important in the accurate management of patient. Contrast enhanced CT with thin multi slice reconstruction and MRCP are non invasive modalities used in demonstrating the fistulous tract. Here we present two cases with their clinical features and radiological findings useful for diagnosing the fistula.
Keywords: Pancreaticopleural fistula; Hemorrhagic pleural effusion; Pancreatitis; Pleural fluid amylase; lipase
Introduction
Pancreatic pleural effusion secondary to fistulous communication between pancreas and pleura is a rare complication of chronic pancreatitis. Patients with fistula tend to have progressive shortness of breath and chest pain out of proportion to abdominal pain. Massive one sided hemorrhagic pleural effusion with raised amylase and protein is highly diagnostic of pancreaticopleural fistula. It is difficult to diagnose and many patients undergo extensive pulmonary investigations before the final diagnosis is reached. So, high index of clinical suspicion and early evaluation of pleural fluid amylase and lipase helps in avoiding the delay in diagnosis. CECT and MRCP are helpful in visualizing the fistulous communication between the pancreatic duct and/or pancreatic pseudocyst and the pleural cavity.
Case Report
Case 1
A 47-year-old male presented with shortness of breath, intermittent hemoptysis and chest pain of 6 months duration. He had a history of pancreatitis 3 years back. A chest radiograph showed massive left sided pleural effusion, for which he underwent intercostal drainage. The pleural fluid was hemorrhagic with amylase level of 6200 U/L (reference range: 0-180 U/L), protein 5 g/dL (reference range: 0-3.5 g/dL) and adenosine deaminase 22 U/L (ADA; reference range: 0-32 U/L). Cytology for malignant cells was negative, gram staining and culture showed no acid fast bacilli. Blood examination showed serum amylase levels of 230 U/L (reference range: 0-100 U/L).
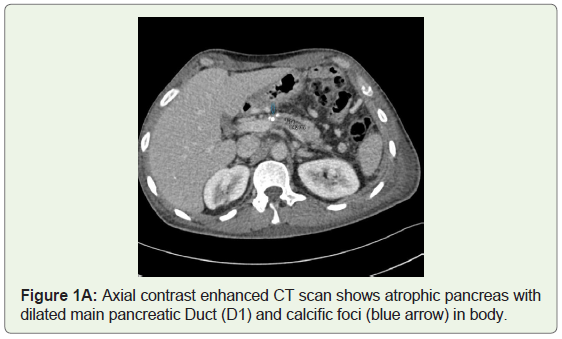
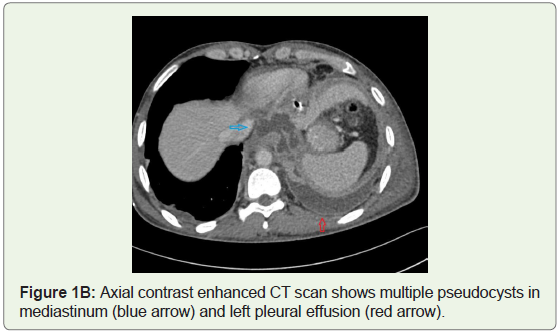
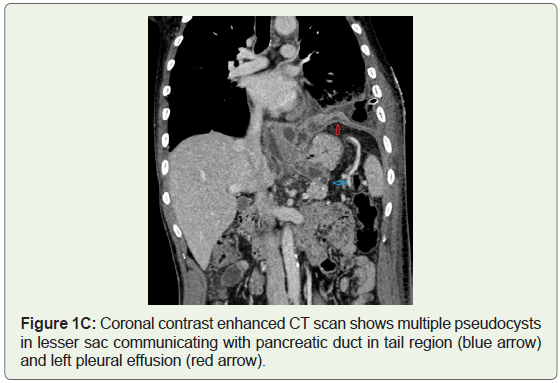
Imaging findings-Contrast enhanced CT study showed moderate left pleural effusion with underlying lung collapse and intercostal drain tube in situ. Pancreas was atrophic with dilated main pancreatic duct (~4mm) and multiple calcific foci in head and body (Figure 1A). Multiple small peripherally enhancing collections were seen in lesser sac and around the esophagus in lower mediastinum communicating with the main pancreatic duct and left pleural space, suggestive of pancreaticopleural fistula (Figure 1B, Figure 1C).
Management-Patient was treated conservatively by intercostal drainage of pleural effusion and administration of octreotide. Post treatment follow up for 6 months revealed no recurrent effusion.
Case 2
A 44-year-old man, with increasing dyspnea, mild epigastric discomfort and anorexia for three months prior to hospitalization, was admitted to our hospital. Past medical history was relevant for chronic alcoholic pancreatitis. Prior to admission, patient had been diagnosed with a left pleural effusion at a district level hospital where he had undergone a therapeutic pleural tap twice and received antibiotics.
Physical examination was suggestive of a notable pleural effusion in the left pleural cavity and only mild pain was elicited on deep palpation in the epigastric region. Laboratory data were as follows: serum amylase 323 U/L (reference range: 8-53 U/L), lipase 516 U/L (reference range: 8-78 U/L) and calcium 7.9 mg/dL (reference range: 9-10.5 mg/dL). No biochemical signs of cholestasis or hepatocellular damage were found.
Chest radiograph in our hospital revealed gross left pleural effusion. Abdominal ultrasound showed an atrophic pancreas and a round fluid collection located in the superior aspect of pancreatic body. Pleural fluid analysis revealed amylase level of 12540 U/L (reference range: 0-180 U/L) and protein 4.7 g/dL (reference range: 0-3.5 g/dL). With the clinical suspicion of a pancreaticopleural fistula, further evaluation by Magnetic Resonance cholangiopancreatography (MRCP) was carried out.
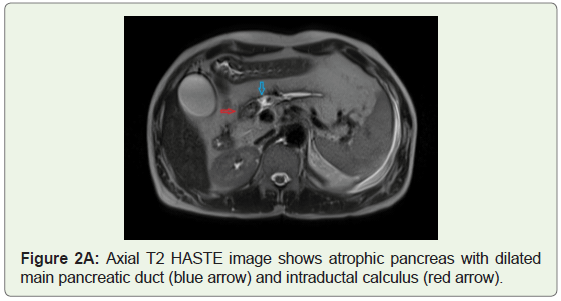
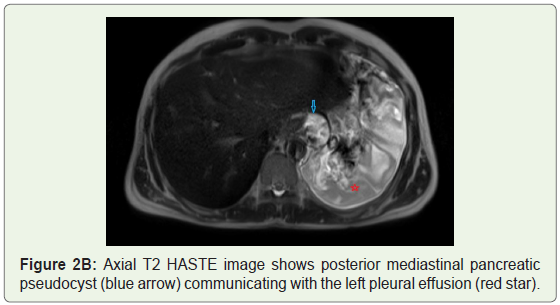
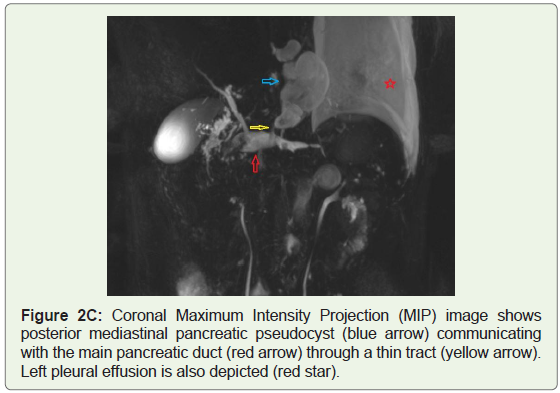
Imaging findings-Abdominal MRCP was performed by a 1.5 T unit with a phased-array body coil. We used heavily T2-weighted sequences: a Half-Fourier Single-shot Turbo spin-Echo (HASTE) 2D breath-hold and 3D respiratory gated Turbo Spin-Echo (TSE) with Multiplanar Reconstruction (MPR) and Maximum Intensity Projection (MIP). The entire pancreatic parenchyma was atrophic and replaced by fat. Main pancreatic duct was dilated with an intraductal hypointense filling defect (measuring ~2.2x1.2cm) in head region, suggestive of calculus (Figure 2A). A lobulated cystic lesion of ~3.3x4.2x5.8cm (mediolateral x anteroposterior x craniocaudal) was seen in the superior aspect of pancreatic body extending into the posterior mediastinum of thorax. It was seen to communicate with the main pancreatic duct and left pleural effusion, suggestive of pancreaticopleural fistula (Figure 2B,Figure 2C).
Management-Intercostal drainage of left pleural effusion was performed. Medical treatment was started with Total Parenteral Nutrition (TPN) and the administration of broad spectrum antibiotics, proton pump inhibitors and octreotide. The patient was discharged without dyspnea or abdominal symptoms in an improved general condition.
Discussion
Pancreaticopleural fistula is a rare but serious complication of acute pancreatitis, more commonly chronic pancreatitis. It is estimated to occur in only 0.4% of patients with chronic pancreatitis and 4.5% of patients with pancreatic pseudocysts. They can also present following surgical pancreatic resections, percutaneous drainage of a pseudocyst and abdominal trauma [1-3]. The most common cause of chronic pancreatitis leading to pancreaticopleural fistula formation is alcohol abuse (around 80%) with gallstone etiology being much less common [4,5].
It falls under the domain of ‘internal pancreatic fistulas’, a term coined by Cameron, et al. and comprises pancreaticopleural fistula and pancreatic ascites [2].
The underlying mechanism of fistula formation involves either a leak or rupture of a pseudocyst, or direct pancreatic duct disruption. If the leak occurs anteriorly, extrapancreatic communication of the pancreatic duct with the peritoneum will result in the formation of a pancreaticoperitoneal fistula, which manifests as ascites. If the disruption occurs posteriorly, pancreatic secretions will enter the retroperitoneum and may dissect through the aortic or esophageal hiatus into the mediastinum. This will either develop into a pancreaticopleural fistula or mediastinal pseudocyst, which in turn will rupture into the pleural cavity to form a pancreaticopleural fistula [3,4,6,7]. On rare occasions, a fistula may also communicate with the pericardium (pancreaticopericardial), tracheo-bronchial tree (pancreaticobronchial) or esophagus (pancreaticoesophageal).
Involvement of the left pleural space is more common accounting for 76% of cases, and pleural effusions tend to be recurrent despite repeated thoracocentesis [6,7]. Involvement of both pleural spaces is less common and has been reported in 14% of patients with pancreaticopleural fistulas.
Males in mid forties with excessive alcohol intake and multiple recurrent episodes of pancreatitis form the classical description of patients who develop pancreaticopleural fistula. Patients typically present with pulmonary symptoms such as dyspnea, cough and chest pain [1]. The diagnosis is often delayed and many patients undergo extensive pulmonary investigations before the final diagnosis is reached. For this reason, pancreaticopleural fistula must be suspected in individuals with recurrent pleural effusions and concomitant history of pancreatitis.
Diagnosis
The single most important diagnostic procedure is a pleural tap to determine the level of pleural fluid amylase. Pleural fluid amylase would be significantly elevated (> 1,000 U/L) with mean amylase levels above 10,000 U/L (13,000-53,000 U/L) in patients with pancreaticopleural fistula [2,8,9].
Pleural effusions with high amylase can also be found in acute pancreatitis, parapneumonic effusion, pulmonary tuberculosis, esophageal perforation, liver cirrhosis, hydronephrosis, leukaemia/lymphoma and malignancies of the lung, pancreas, rectum, and in females, the gynaecological system. However only pancreaticopleural fistula results in pleural fluid amylase levels above 50,000 U/L [3,8,10]. The pleural fluid protein level would also be high (> 30 g/L) due to chronic inflammation of the pleural surface [10].
Once elevated amylase levels from a diagnostic pleural tap confirms the suspicion of a pancreaticopleural fistula, several imaging modalities are available for visualization of the fistula. CT, ERCP and MRCP are most widely used in current practice, and the sensitivity of each modality in detecting pancreaticopleural fistula is 47%, 78% and 80% respectively [8,11]. Sensitivity of CT is less, but it is useful in demonstrating pancreatic parenchymal atrophy, calcification, duct dilatation and pseudocysts.
ERCP used to be the preferred investigation for confirming the diagnosis of pancreaticopleural fistula. It can directly visualize the papilla and its adjacent anatomy and has the additional advantage of performing endoscopic therapeutic maneuvers. However, ERCP has its shortcomings; it is invasive in nature and unable to clearly demonstrate a fistula if the site of ductal disruption occurs distal to stricture [5,12,13]. Risk of potentially life-threatening complications such as infection, pancreatitis, bleeding and perforation is also present [9]. The use of ERCP as a first-line tool for confirmation of pancreaticopleural fistula is discouraged in view of its limitations. Currently, MRCP appears to be the imaging modality of choice due to its noninvasive nature and ability to visualize a fistula beyond strictures. In addition, it is very useful in depicting pancreatic parenchymal and ductal structural changes, as well as the presence of small intra- or extrapancreatic pseudocysts and peripancreatic collections [5]. It is considered superior to CT in identifying a fistula in the pancreatic region and its noninvasiveness is advantageous as compared to ERCP. Treatment options include somatostatin analogues, thoracocentesis, Endoscopic Retrograde Cholangiopancreatography (ERCP) with pancreatic duct stenting and surgery.
Conclusion
Pancreaticopleural fistula is rare and should be suspected when patient presents with multiple recurrent episodes of pancreatitis with excessive alcohol intake and on imaging showing massive one sided pleural effusion with coexistent features of chronic pancreatitis. Elevated pleural fluid amylase, lipase and high protein levels will further help in diagnosing the condition. Chest radiograph, ultrasound of abdomen followed by MRCP forms ideal imaging protocol for accurate evaluation of pancreaticopleural fistula. The recommended treatment options include octreotide, thoracocentesis and ERCP with/without endoscopic pancreatic stent placement. Surgery carries a significant mortality risk and is reserved for those who do not respond to medical management or develop complications.
References
- Pandey S, Shetty SA, Janarthanan K, Balalakshmoji D, Sen KK, et al. (2014) Pancreatico-pleural and bronchial fistulae and associated pseudocysts: case series. JOP 15: 478-484.
- Wronski M, Slodkowski M, Cebulski W, Moronczyk D, Krasnodebski IW (2011) Optimizing management of pancreaticopleural fistulas. World J Gastroenterol 17: 4696-4703.
- Vyas S, Gogoi D, Sinha SK, Singh P, Yadav TD, et al. (2009) Pancreaticopleural fistula: an unusual complication of pancreatitis diagnosed with magnetic resonance cholangiopancreatography. JOP 10: 671-673.
- Dhebri AR, Ferran N (2005) Nonsurgical management of pancreaticopleural fistula. JOP 6: 152-161.
- Rockey DC, Cello JP (1990) Pancreaticopleural fistula. Report of 7 patients and review of the literature. Medicine (Baltimore) 69: 332-344.
- King JC, Reber HA, Shiraga S, Hines OJ (2010) Pancreatic-pleural fistula is best managed by early operative intervention. Surgery 147: 154-159.
- Sut M, Gray R, Ramachandran M, Diamond T (2009) Pancreaticopleural fistula: a rare complication of ERCP-induced pancreatitis. Ulster Med J 78: 185-186.
- Ali T, Srinivasan N, Le V, Chimpiri AR, Tierney WM (2009) Pancreaticopleural fistula. Pancreas 38: e26-e31.
- Oh YS, Edmundowicz SA, Jonnalagadda SS, Azar RR (2006) Pancreaticopleural fistula: report of two cases and review of the literature. Dig Dis Sci 51: 1-6.
- Ondrejka P, Faller J, Siket F, Tóth G, Sugár I, et al. (2000) Isolated massive pleural effusion caused by pancreatico-pleural fistula. Z Gastroenterol 38: 583-585.
- Zubiaurre L, Oyarzabal I, Berguiristain A, Amato E, Zapata E, et al. (2005) Fistula pancreaticopleural: pruebas diagnósticas y tratamiento. Cir Esp 77: 313-371.
- Monteiro E, Terra JCA, Figueiredo LBP, Miranda LHS (2002) Pseudocisto de pâncreas associado a derrame pleural maciço. J Pneumologia 28: 159-162.
- Ribeiro B, Gomes D, Rosa A, Amaro P, Tomé L, et al. (2000) Derrame pleural recidivante por fístula pancreático-pleural. Journal Português de Gastroenterologia 7: 161-164.