Case Report
Clinico-Radiological Presentation ofCerebrotendinous Xanthomatosis (CTX) in Two Sisters of an Indian Family with Review of Literature
Pasha SA1*, Padmaja2, Nageswara Rao T3, Sathish G4 and Bhaskara Rao B5
1Associate professor of Neurology in NRI Medical college and General Hospital, Chinakakani, Guntur, Andhra Pradesh, 522 503, India
2Associate Professor of Radiology, NRI Medical college and General Hospital, Chinakakani, Guntur, Andhra Pradesh, 522 503, India
3Professor of Radiology, NRI Medical college and General Hospital, Chinakakani, Guntur, Andhra Pradesh, 522 503, India
4Postgraduate in General Medicine, NRI Medical college and General Hospital, Chinakakani, Guntur, Andhra Pradesh, 522 503, India
5Professor of Medicine, NRI Medical college and General Hospital, Chinakakani, Guntur, Andhra Pradesh, 522 503, India
Corresponding author: Shaik Afsar Pasha, Department of Neurology, Chamber no: 278, NRI Medical collegeand General Hospital, Chinakakani, Guntur, Andhra Pradesh, 522 503, India, Tel: 09989361983; E-mail: afsarpasha81@gmail.com
Citation: Pasha SA, Padmaja, Rao TN, Sathish G, Rao BB. Clinico-Radiological Presentation of Cerebrotendinous Xanthomatosis (CTX) in Two Sisters 02 of an Indian Family with Review of Literature. Indian J Appl Radiol. 2017;3(1): 111.
Copyright © 2017 Pasha SA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Applied Radiology | Volume: 3, Issue: 1
Submission: 12/11/2016; Accepted: 03/02/2017; Published: 06/02/2017
Abstract
Cerebrotendinous Xanthomatosis (CTX) is an autosomal recessively inherited, treatable, metabolic lipid storage disorder, presenting with early nonneurological manifestations (intellectual disability, chronic intractable diarrhea, juvenile bilateral cataracts, multiple xanthomata around the eyelids and Achilles tendons, premature atherosclerosis and pulmonary dysfunction) followed several years later by adult-onset neurological dysfunctions (dementia, spasticity, ataxia, peripheral neuropathy) and neuropsychiatric symptoms. We are presenting two siblings of a family with similar clinical phenotype. Diagnosiswas made on clinico-radiological grounds followed by confirmation of xanthomata in histopathological examination. This case presentation widens the clinical and radiological spectrum (MRI brain and spine) of CTX and will be discussing in-detail about the differential diagnosis. This report highlights the importance of early diagnosis of a rare inherited treatable metabolic disorder so as to prevent the lethal complications.
Introduction
Cerebrotendinous Xanthomatosis (CTX) is a rare, autosomalrecessively inherited disorder of bile acid biosynthesis due to mutation of hepatic mitochondrial enzyme CYP27A1gene, coding for a sterol 27-hydroxylase which normally catalyzes the oxidation of cholesterol to bile acids, on chromosome 2q33-qter, leading to increased deposition of cholesterol and cholestanol in multiple tissues namely central and peripheral nervous system, soft tissues, lens of the eyes, cardiovascular system, lungs, liver and kidneys [1]. Clinicallycharacterized by progressive dementia, ataxia, spasticity, peripheralneuropathy, accompanied by tendon xanthomas, pre-senile cataracts,premature atherosclerosis and pulmonary dysfunction [2,3]. Early diagnosis is very important, as it is treatable and sometimes reversible. Although reported from many parts of the world, reports from India are rare. We are reporting two cases of CTX.
Case 1 (Index Case)
A 47 year old lady, fourth of five siblings born of consanguinousmarriage, suffering from 9 year history of chronic progressive unsteadiness of gait while passing through the narrow passages and was swaying to either side while walking and it did not vary with darkness. She was dull, apathetic, a motivational and withdrawn for 8 years with occasional suicidal thoughts. She was unable to cope up with peers and her scholastic performance was poor. History of tightness and stiffness of the lower limbs were present. History of chronic diarrhoea since 8 years of age, not responding to the usual probiotics. Underwent cataract extraction with lense implantation at 17 years of age. Since 27 years of age noticed multiple swellings started on the left ankle followed by Right Ankle, eyes and nose. Patient`s younger sister was suffering from similar illness.
She was seen by Paediatrician at 3 years of age for delayed motor skills and reassured. At seventeen years of age, bilateral cataractsurgery was done by an ophthalmologist. At 40 years of age, left ankleswelling was excised by a General Surgeon which recurred. She had been using homeopathy, ayurveda drugs for 30 years.
On general examination she was short statured (143 cms), Body Mass Index (BMI) of 24.94 with bilateral pescavus with hammer toes, multiple globular swellings over the sides of the bridge of the nose and bilateral Achilles tendons (Figures 1A-1D and Figures 2A-2D). Skin examination showed planar xanthoma.
On neurological examination she was conscious, disoriented to time and place and familiar relatives with scoring of 12/28 on Mini Mental Status Examination (MMSE-Folstein) - suggestive of severe dementia. Bilateral pseudophakia, with amyotrophy of bilateral hands with clawing of fingers, minimal spasticity of all four limbs, with distal weakness of hands and feet. She had brisk tendon jerks with bilateral Babinsky`s. Gait cycle showed wide based stance associated with swaying and dragging of feet. Allied reflexes like Hoffman,Wartenberg`s were present. Primitive glabellar reflex was present suggestive of neurodegeneration. Significant cerebellar damage was evident through bilateral impaired finger nose ataxia, intentional and kinetic tremors of the hands, Rebound phenomena of the hands, stance ataxia, and severe Gait ataxia. Romberg`s test was positive, vibration sense lost below knee joint in both lower limbs suggestive of large fibre peripheral neuropathy.
Case 2
Her sibling of age 49 years, had the almost similar clinicalphenotype with predominant appendicular ataxia, dementia, peripheral neuropathy with spasticity, juvenile cataracts except diarrhoea. She had osteoporosis induced pathological fractures and hypothyroidism with normal blood cholesterol in addition. Laboratory evaluation in case1 showed hypercholesterolemia (220 mg/dl) with hyper triglyceridemia (369 mg/dl) with LDL: HDL of 3.1 while there was normal cholesterol and elevated TSH of 6.25 micro/ml suggestive of hypothyroidism in case 2. Cardiac screening was normal in both cases.
Histopathology of the tendon swellings from right ankle under haematoxylin and eosin revealed disruption of fibrous collagenous bands of the tendon by masses of Xanthomatous cells containing foamy cytoplasm amassed around cholesterol clefts and multinucleated giant cells, confirming the Xanthomatous tissue (Figures 3A-3B).
Imaging Findings
MRI Brain in the two cases revealed symmetrical T2 and FLAIRhyperintensities in bilateral dentate nuclei of cerebellum with foliarprominence with dilation of fourth ventricle suggesting cerebellaratrophy. Bilateral pyramidal tracts were hyperintense along the posterior limb of internal capsule and crus cerebri on T2 and FLAIR sequences (Figures 4A-4D and Figures 5A-5D). In Case 2 it additionally revealed T2 hypointense lesions in the choroid plexus of bilateral trigone of lateral ventricles suggestive of “choroid plexus xanthogranulomas” (Figure 5C). Careful soft tissue examination showed xanthomas of bilateral lower eyelids in case 2 and left lower lid in index case (Figure 4C and Figure 5B). MRI spine showed normal spinal cord with right gluteal xanthomas which were T1 and T2 hypointense in Case1 (Figure 5D,Figure 5E).
Figure 5: a-b axial T2wMRI and FLARI sequence of Brain of Case 2 showing hyperintensity of dentate nuclei with foliar prominence of cerebellum (arrow head), c- axial T2 wMRI of Brain showing choroid plexus xanthogranuloma (arrow head), d-coronal T2 wMRI of Brian showing pyramidal tract hyperintensity (arrow head).
MRI of ankles showed bulky achilles tendons with convexanterior margin, well defined heterogenous (iso to hypointense onT1, T2 and STIR relative to adjacent tendons) signal intensity lesionin the distal part of achilles tendon suggestive of Achilles tendonXanthoma (Figures 6A-6E).
Discussion
Earliest reports of CTX was made by Bogaert’s in 1937 followed by few hundred cases worldwide [4,5]. There are no consensus data on the prevalence of CTX, the estimated rate being <5/100000 worldwide. Most patients were traced to Israel, Netherlands, and USA. From India, Sodhi et al. documented the first case of CTX in 1973 [6]. Subsequently by Nair et al. from Trivandrum [7].
CTX can present to different specialists because of its multisysteminvolvement. It may manifest in neonates and in early childhood with chronic diarrhea, congenital or juvenile cataract, delayed developmental milestones, mental retardation and occasionally, neonatal cholestatic jaundice. The typical triad of neurological dysfunction, tendon xanthoma, and early onset cataract is the clinical hallmark. This is often not found on first contact with specialist. Bordia and Saifee from India reported oro-mandibular dyskinesia as the presenting feature of CTX which was seen at first by dentist [8]. CTX shares presence of xanthoma and premature atherosclerosis with other lipid storage disorders including familial hyper cholesterolemia and sitosterolemia. Progressive neurological dysfunction and early cataract are seen in CTX only.
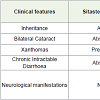
The presented cases highlighted the classical manifestations ofCTX in the form of progressive dementia, pyramidal, cerebellar,peripheral neuropathy in association with bilateral cataracts, tendonand eyelid xanthomas on a background of chronic diarrohea. Case 2, also had hypothyroidism, osteoporosis induced pathological fractures. The clinical syndrome may include other neurological features like fronto-temporal dementia [9,10], extra pyramidal symptoms, including dystonia and oromandibular dyskinesia [8], early-onset Parkinson disease [11], seizures [12], muscular symptoms like myopathic facies [13] (Table 1).
According to the clinical suspicion index of Mignarri et al. for CTX, where our both cases had all the four clinical features evolved in the same order as described like diarrohea, presenile cataracts, xanthomas and neurological abnormalities [14].
Soffer and colleagues [15] demonstrated that the parenchymal destruction in the brain starts in the white matter with cholestanol cumulation and progresses in a centrifugal manner with axonalspheroids being more marked in the brainstem with decreasing order of severity in the centrum semiovale. The presenile cataracts of CTX contain high cholestanol compared to the cholesterol of senile cataracts.
Earliest and most important abnormalities are noted in the cerebellum with high signal of deep gray nuclei namely dentate nuclei with occsaional hypointensity. Sometimes white matter lesions are surrounded by rim of hypointensity in T2 weighted images suggestive of macroscopic xanthomata, calcium or hemosiderin deposits. Neuro-imaging modalities demonstrate diffuse atrophy of the brain, as well as focal lesions (including demyelinating lesions and, rarely, xanthomata) in the cerebellum, basal ganglia, and cerebrum. CT scan is less sensitive but MRI abnormalities are obvious. Typical patterns on MRI brain include bilateral lesions consistent with a metabolic abnormality. Destefano et al. had reported T2 hyperintensity of the dentate nuclei as an earliest and characteristic finding of CTX in their 79% of patients [16]. T2 abnormalities are also found in the globus pallidus, substantia nigra, and inferior olives with extension into the surrounding white matter with sparing of the U fibers and the corpus callosum in later years of the disease. Hence CTX should be considered in the differential diagnosis of leukodystrophies [17].
Focal lesions in the brain involving the corona radiata, centrumsemiovale, globus palldum [18,19], and posterolateral columns of spinal cord [19] are described and on the other hand brainstem, corpus callosum [19] and atrophy of spinal cord [20], have been reported.
Choroid plexus xanthogranulomas are benign tumors composed of xanthoma cells (macrophages), cholesterol clefts, chronic inflammatory cellular reaction, and hemosiderin. At autopsy series they have been found incidentally in 1.6-7% of cases [21]. These lesionsare most commonly seen bilaterally in the lateral ventricles; they areasymptomatic because they are too small to obstruct the ventricles. However, those occurring in the third ventricle are more likely to present with non-communicating hydrocephalus. Hypointensity on T2 weighted MR sequence is classical of xanthomatous tissue. Similardemonstration of bilateral choroid plexus xanthogranuloma in a patient with CTX was reported by Fiorelli et al. [22].
Magnetic resonance spectroscopy reveals diffuse mitochondrial dysfunction and axonal damage, with large amounts of lactate and decreased N -acetylaspartate in the periventricular white matter andcerebellar hemispheres [16]. Similar findings can as well be reflected in the affected xathomatous tissues.
Isolated spinal cord white matter disease has been described [20-23]. MRI may reveal increased intensity in the lateral and dorsal columns, even in mainly cerebral forms of the disease[16]. Magnetization transfer imaging has been found to be a reliable quantitative indicator of the extent of damage in the brain parenchyma [23]. MRI can also be used to evaluate possible tendon xanthomata outside the central nervous system; enlargement of the tendons and xanthomas of eyelids as evident in our case.
Treatment of this disease includes the combination of CDCA (300mg/day) and HMG Co A inhibitor (Simvastatin/Pravastatin 10 mg/ day) is more effective in reducing cholestanol levels and normalizing LDL cholesterol [24,25], LDL pheresis, and dietary modifications. The results of treatment are variable, there was either arrest of the disease progression or partial improvement of clinical, biochemical, and MRI abnormalities. Genetic analysis is important in identifying the carriers of the disease. Early institution of CDCA therapy can prevent development of CTX phenotype. It improves bile acid metabolism and decreases cholestanol levels. The drug CDCA is not available in India and is very expensive.
Conclusion
Being a multisystemic disease, high index of suspicion is required among the specialities to diagnose CTX whenever patients presentwith mental retardation, presenile cataract, intractable diarrhoea with or without neurological involvement. Imaging abnomralities are numerous and almost speculate the pathology of the underlying disease. After significant disease progression, treatment does not readily reverse neurological deficits that have already occurred.
References
- Cali JJ, Hsieh CL, Francke U, Russell DW (1991) Mutations in the bile acid biosynthetic enzyme sterol 27-hydroxylase underlie cerebrotendinous xanthomatosis. J Biol Chem 266: 7779-7783.
- Federico A, Dotti MT (2003) Cerebrotendinous xanthomatosis: clinical manifestations, diagnostic criteria, pathogenesis, and therapy. J Child Neurol 18: 633-638.
- Moghadasian MH, Salen G, Frohlich JJ, Scudamore CH (2002) Cerebrotendinous xanthomatosis: a rare disease with diverse manifestations. Arch Neurol 59: 527-529.
- Gallus GN, Dotti MT, Federico A (2006) Clinical and molecular diagnosis of cerebrotendinous xanthomatosis with a review of the mutations in the CYP27A1 gene. Neurol Sci 27: 143-149.
- Bjorkhem I, Hansson M (2010) Cerebrotendinous xanthomatosis: an inborn error in bile acid synthesis with defined mutations but still a challenge. Biochem Biophys Res Commun 396: 46-49.
- Sodhi HS, Agnish ND, Khudchedkar BJ (1973) Cholestanol biosynthesis in cerebrotendinous xanthomatosis. Neurology Bombay 4: 657.
- Nair KR, Jose J, Kunju M, Iype M (1994) Cerebrotendinous xanthomatosis. J Assoc Physician India 42: 491-492.
- Bordia S, Saifee AA (2003) Cerbrotendinous xanthomatosis with oromandibular dyskinesia. Neurol India 51: 556-558.
- Sugama S, Kimura A, Chen W, Kubota S, Seyama Y, et al. (2001) Frontal lobe dementia with abnormal cholesterol metabolism and heterozygous mutation in sterol 27-hydroxylase gene (CYP27). J Inherit Metab Dis 24: 379-392.
- Guyant-Maréchal L, Verrips A, Girard C, Wevers RA, Zijlstra F, et al. (2005) Unusual cerebrotendinous xanthomatosis with fronto-temporal dementia phenotype. Am J Med Genet A 139: 114-117.
- Dotti MT, Federico A, Garuti R, Calandra S (2000) Cerebrotendinous xanthomatosis with predominant parkinsonian syndrome: further confirmation of the clinical heterogeneity. Mov Disord 15: 1017-1019.
- Koyama S, Kawanami T, Tanji H, Arawaka S, Wada M, et al. (2012 ) A case of cerebrotendinous xanthomatosis presenting with epilepsy as an initial symptom with a novel V413D mutation in the CYP27A1 gene. Clin Neurol Neurosurg 114: 1021-1023.
- Dotti MT, Manneschi L, Federico A (1995) Mitochondrial enzyme deficiency in cerebrotendinous xanthomatosis. J Neurol Sci 129: 106-108.
- Mignarri A, Gallus GN, Dotti MT, Federico A (2014) A suspicion index for early diagnosis and treatment of cerebrotendinous xanthomatosis. J Inherit Metab Dis 37: 421-429.
- Soffer D, Benharroch D, Berginer V (1995) The neuropathology of cerebrotendinous xanthomatosis revisited: a case report and review of the literature. Acta Neurophthol 90: 213-220.
- De Stefano N, Dotti MT, Mortilla M, Federico A (2001) Magnetic resonance imaging and spectroscopic changes in brains of patients with cerebrotendinous xanthomatosis. Brain 124: 121-131.
- Androdias G, Vukusic S, Gignoux L, Boespflug-Tanguy O, Acquaviva C, et al. (2012) Leukodystrophy with a cerebellar cystic aspect and intracranial atherosclerosis: an atypical presentation of cerebrotendinous xanthomatosis. J Neurol 259: 364-366.
- Dotti MT, Federico A, Signorini E, Caputo N, Venturi C, et al. (1994) Cerebrotendinous xanthomatosis(van Bogaert-Scherer-Epstein disease): CT and MR findings. AJNR Am J Neuro radiol 15: 1721-1726.
- Barkhof F, Verrips A, Wesseling P, van Der Knaap MS, Van Engelen BG, et al. (2000) Cerebrotendinous Xanthomatosis: The spectrum of imaging findings and the correlation with neuropathologic findings. Radiology 217: 869-876.
- Verrips A, Nijeholt GJ, Barkhof F, Van Engelen BG, Wesseling P, et al. (1999) Spinal xanthomatosis: a variant of cerebrotendinous xanthomatosis. Brain 122: 1589-1595.
- Pear BL (1984) Xanthogranuloma of the choroid plexus. AJR 143: 401-402.
- Fiorelli M, Di Piero V, Bastianello S, Bozzao L, Federico A (1990) Cerebrotendinous xanthomatosis: clinical and MRI study: (a case report). J Neurol Neurosurg. Psychiatry 53: 76-78.
- Inglese M, De Stefano N, Pagani E, Dotti MT, Comi G, et al. (2003) Quantification of brain damage in cerebrotendinous xanthomatosis with magnetization transfer MR imaging. AJNR Am J Neuroradiol 24: 495-500.
- Kuriyama M, Tokimura Y, Fujiyama J, Utatsu Y, Osame M (1994) Treatment of cerebrotendinous xanthomatosis: effects of chenodeoxycholic acid, pravastatin, and combined use. J Neurol Sci 125: 22-28.
- Verrips A, Wevers RA, Van Engelen BG, Keyser A, Wolthers BG, et al. (1999) Effect of Simvastatin in addition to Chenodeoxycholic acid in patients with cerebrotendinous xanthomatosis. Metabolism 48: 233-238.