Research Article
Role of B-Scan in Cataract Patients
Atula Jain*, Neelam Gauba, Inderjit Kaur, Sohan Singh and Happy Jaswal
Department of Radio Diagnosis and Imaging, Government Medical College, Amritsar, 143001. Punjab, India
Corresponding author: Atula Jain, Department of Radio Diagnosis and Imaging, Government Medical College, Amritsar, 143001. Punjab, India, E-mail: atula_unique13@yahoo.co.in
Citation: Jain A, Gauba N, Kaur I, Singh S, Jaswal H. Role of B-Scan in Cataract Patients. Indian J Appl Radiol. 2017;3(1): 110.
Copyright © 2017 Jain A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Applied Radiology | Volume: 3, Issue: 1
Submission: 27/12/2016; Accepted: 24/01/2017; Published: 25/02/2017
Abstract
Aim: The purpose of the study is to evaluate posterior segment lesions with B-scan ultrasound in pre-operative cataract patients.
Materials and methods: The present study was conducted on 100 cataract patients referred from outpatient departments who were evaluated for posterior segment lesions with high resolution ultrasonography.
Results: of the total 100 patients, 52 were male and 48 were female. The study population (100 cases) was divided into two groups; 1) traumatic cataract: 18(18%) patients and 2) non traumatic cataract: 82(82%) patients. Among 18 patients of traumatic cataract, following posterior segment pathologies were noted in 6(33.33%) patients, Retinal Detachment (n=2), Vitreous Haemorrhage (n=1), Intraocular Foreign Body (n=3), and no posterior segment pathology was noted in 12(66.67%) patients. Among 82 patients of non traumatic cataract following posterior segment pathologies were noted in 8patients: Retinal Detachment (n=3), Vitreous Haemorrhage (n=2), Posterior Vitreous Detachment (n=1), Posterior Staphyloma (n=2) patients and no posterior segment pathology was noted in 74(90.24%) patients. Posterior segment pathologies on B-scan tended to occur significantly more frequently in patients with diabetes mellitus (OR=12.03, P=0.002). On the other hand, Hypertension (OR=1.72, P=0.53) and smoking (OR=2.67, P=0.41) were not significantly associated with posterior segment pathology on B-scan.
Conclusion: It was concluded that B-scan is a good modality for diagnosing posterior segment pathologies in cataract patients and thus helps in predicting the visual prognosis.
Keywords: B-scan; Ultrasound; Posterior segment pathology; Cataract
Introduction
The most recent estimates from WHO reveal that 47.8% of global blindness is due to cataract and in South Asia region which includes India, 51% of blindness is due to cataract. Cataract surgery has been viewed as one of the most cost-effective health interventions. Cataract has been documented to be the most significant cause of bilateral blindness in India. India is committed to the goal of elimination of avoidable blindness by 2020 in line with the Global Vision 2020: the right to sight initiative [1].
Cataract is defined as an opacity of any portion of the lens, regardless of visual acuity [2]. Many of these cases have advanced cataracts that preclude visualization of fund us prior to cataract surgery. Such visualization is considered important to provide accurate prognosis for vision after cataract surgery. Under such circumstances ultrasonographic examination might provide information regarding such abnormalities [3]. Surgery for traumatic cataracts is a potentially complex procedure. Careful ophthalmic imaging using ultrasound may result in finer pre-operative detail regarding lens support structures, and may therefore give the surgeon the advantage when planning surgery [4].
Ultrasound is a safe technique, cheaper, easily available and provides more affordability compared to other imaging techniques such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) [5]. Ultrasound is an acoustic wave that consists of an oscillation of particles within a medium. Dynamic scanning is essential for differentiation between retinal detachment and vitreous membranes or tumour and haemorrhage. X-rays can detect only radiopaque foreign bodies and will miss radioloucent ones. B-scan offers a more accurate localisation of the foreign body, especially in relation to the ocular wall.
Ultrasound was first used in ophthalmology in 1956 by the American ophthalmologists, Mundt and Hughes [6]. They used A-scan mode to evaluate an intraocular tumour. B-scan was introduced in ophthalmic practice by Baum and Greenwood in 1958 [7]. However, it was not until 1972, when Bronson and Turner produced the first contact B-scan method, that ultrasonography became a more practical investigation [8]. B-scan (brightness) mode is more useful than A (Amplitude) scan for a better demonstration of the shape and topographic relationship of lesions in the posterior segment [5].
The purpose of the study is to visualise the status of posterior segment with B-scan ultrasound in pre-operative cataract patients in order to evaluate posterior segment pathologies.
Aims and Objectives
To evaluate the prevalence and nature of posterior segment pathologies detected by B-scan ultrasound in pre-operative cataract patients and to study various patient risk factors that increase the likelihood of posterior segment pathology. The objective of this study is to help the ophthalmologic surgeon in predicting possible visual prognosis in addition to proper planning and execution of surgery and to decide postoperative management.
Materials and Methods
The present study was conducted in a tertiary care teaching hospital on 100 patients referred from outpatient departments by ophthalmologists and provisionally diagnosed as cataract patients. Patients of all age groups and both sex having cataract were included in the study. Each patient was subjected to detailed history, local examination and B-scan ultrasound. The patients were made to lie supine on the examination table. They were evaluated using e-saote ultrasound machine and PhilipsHD11XE machine both equipped with a real- time linear high-frequency probe of 7-12 MHZ placed in Radio diagnosis department and with P60 Ultrasonic Bio microscope (with Paradigm Dicon) equipped with 12.5 MHZ probe placed in Ophthalmology department. Contact method of examination was used. The probe was placed over the closed eyelid after application of coupling gel. B-scan pictures were obtained in axial, transverse and longitudinal sections. The lowest possible decibel gain consistent with the maintenance of adequate intensity was used to optimize the resolution of images.
Observations: Of the total 100 patients, sex wise distribution was 52(52%) patients were male and rest 48(48%) were females. Population wise distribution included 47(47%) patients of rural background and rest 53(53%) patients of urban background.
On the basis of cause of cataract the study population (100 cases) was divided into two groups; 1) traumatic cataract: 18(18%) patients and 2) non traumatic cataract: 82(82%) patients.
Age profile in traumatic cataract patients was as follows; a) 10-20 years: 10(55.55%) patients, b) 21-30 years: 1(5.56%) patient, c) 31-40 years: 2(11.11%) patients, d) 41-50 years: 1(5.56%) patient, e) 51-60 years: 2(11.11%) patients, f) 61-70 years: 2(11.11%) patients, g)>70 years: 0 patient.
Age profile in non traumatic cataract patients was as follows; a) 10-20 years: 0 patient, b) 21-30 years: 1(1.22%) patient, c) 31-40 years: 4(4.88%) patients, d) 41-50 years: 13 (15.85%) patients, e) 51-60 years: 54(65.85%) patients, f) 61-70 years: 9(10.98%) patients, g)>70 years: 1(1.22%) patient.
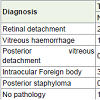
pathology was noted in 6 (33.33%) patients and no posterior segment pathology was noted in 12(66.67%) patients. Posterior segment pathologies observed by B-scan were as follows; a) Retinal Detachment: 2(11.11%) patients, b) Vitreous Haemorrhage:1(5.55%) patient, c) Posterior Vitreous Detachment : 0 patient, d) Intraocular Foreign Body:3(16.67%) patients, e) Posterior Staphyloma: 0 patient.
Among 82 patients of non traumatic cataract, posterior segment pathology was noted in 8(9.76%) patients and no posterior segment pathology was noted in 74(90.24%) patients. Posterior segment pathologies observed by B-scan were as follows; a) Retinal Detachment: 3(3.66%) patients, b) Vitreous Haemorrhage: 2(2.44%) patient, c) Posterior Vitreous Detachment: 1(1.22%) patient, d) Intraocular Foreign Body: 0 patient, e) Posterior Staphyloma: 2(2.44%) patients Table 1 (Below). Representative examples of some of the patients diagnosed by ultrasound are depicted by Figures 1-7 (Below).
Figure 4: Posterior Vitreous Detachment: B-scan shows an echogenic membrane in posterior half of vitreous cavity concentric to globe infront of retino choroidoscleral complex with clear sub vitreal space which does not show any attachment to optic nerve head with high mobility and distinct after movements on dynamic scan.
Discussion
Traumatic cataract was more common in younger age group due to more involvement in outdoor games and activities and thus having more chances of trauma. Non traumatic cataract was most common in 41-60 years as this is the age group for senile cataract. The most common clinical symptom amongst patients included in the study was decreased vision followed by glare, colored halos and the least common was second sight. In case of traumatic cataract patients, trauma was documented in the past history. Posterior segment pathologies in our study were observed in 14 patients (14%) out of 100 patients amongst which 6(6%) patients were of traumatic cataract and 8(8%) patients were of non traumatic cataract.
Another study done by Qureshi et al. in non-traumatic cataract patient group observed that b-scan ultrasound detected retinal detachment in 1.47%, vitreous hemorrhage in 1.91%, posterior vitreous detachment in 1.03%, posterior staphyloma in 1.32%, and no pathology in 93% patients [5]. We observed little high incidence of retinal detachment and posterior staphyloma in our study i.e. 3.65% and 2.44% as compared to 1.47% and 1.32% respectively in their study. No pathology was observed by us in 90.24% patients as compared to their in 93%. Posterior vitreous detachment incidence was almost same in broad context. In traumatic cataract patient group, Quereshi et al. observed retinal detachment in 21.22% patients, vitreous hemorrhage in 15.49%, posterior vitreous detachment in 9.86%, intraocular foreign body in 8.45% and no pathology in 45% patients. In this group they observed high incidence of all compared pathologies except intraocular foreign body. This variation in result could be explained due to the high number of patients i.e. 750 included in their study.
In a study by Anteby et al. in non-traumatic cataract group retinal detachment was observed in 3.9%, vitreous hemorrhage in 2.5% and posterior staphyloma 7.6% [9]. Only posterior staphyloma was observed in high incidence as compared to our observation, i.e. 7.6% vs 2.44%. In traumatic cataract group in the same study retinal detachment observed was 14.8%, vitreous hemorrhage 3.7% and intraocular foreign body in 7.4%. We observed retinal detachment in 11.11%, vitreous hemorrhage in 5.55% and intraocular foreign body in 16.66% in traumatic cataract group. There was large difference in incidence of foreign body in our study.
In another study done by Mendes et al. out of 289 patients with medium to profound opacity of the lens 77.5% presented with vitreous detachment [2]. In 30.1% of the patients, the ultrasound revealed eye abnormalities that could compromise the function of the eye after surgery. The most common of these abnormalities was vitreous opacities (12.1%) followed by retinal detachment (9.3%). Our study observations were markedly less than these observations which could be due to the fact that they examined the patients evaluated during cataract campaigns and they did not take into account separately the patients with or without the history of trauma.
We also studied diabetes mellitus, hypertension and smoking as risk factors for posterior segment pathology in non traumatic cataract patients. In these patients 49(59.76%) out of 82 patients had no apparent risk factor for posterior segment pathology on B-scan. Among the patient risk factors studied, diabetes mellitus was present in 14 patients (17%), hypertension was present in 14 patients (17%) and smoking was present in 5 patients (6.1%). Posterior segment pathologies on B-scan tended to occur significantly more frequently in patients with diabetes mellitus (OR=12.03, P=0.002). Hypertension (OR=1.72, P=0.53) and smoking (OR=2.67, P=0.41) were not significantly associated with posterior segment pathology on B-scan.
Another study done by Amjad et al. observed the patient risk factors in cataract patients. He observed cataract in young age in 67 patients (17%), diabetes mellitus in 21 patients (5.3%), hypertension in 11 (2.8%) [3]. Abnormal posterior segment findings on ultrasound tend to occur significantly more frequently in patients with diabetes mellitus (OR= 4.9, P = 0.003) and younger age (OR= 15.4, P = 0.001). Systemic hypertension (OR= 1.9, P = 0.35) and bilateral advanced cataracts (OR = 1.7, P = 0.17) were not significantly associated with posterior segment pathology on ultrasonography. Similarly we also found increased incidence of diabetes mellitus in cataract patients with posterior segment pathology.
Kalpna et al. in their study found that there were 77(8.1%) patients with diabetes mellitus and cataract who required postsurgical management in vitreo-retinal department [10]. Abnormal posterior segment was seen to occur significantly in patients with diabetic retinopathy (p value=0.036), and hypertensive retinopathy (p value=0.368). We also established the relationship of diabetes as risk factor in cataract patients with posterior segment pathology but no such relationship is established with hypertension in our study. Chanchalani et al. in their study observed 19.6% patients were having ocular and systemic risk factors like hypertension, diabetes, raised intraocular pressure, uveitis and myopia [11]. Among the clinical and systemic features in patients studied in their setup, diabetes mellitus and young age were associated with a greater incidence of abnormalities on B- scan.
We were not able to diagnose central or branch retinal vein occlusion, macular hole, age related macular degeneration, optic atrophy, few cases of diabetic retinopathy and glaucomatous cupping in cataractous patients on B-scan ultrasound resulting in poor visual outcome after surgery. Therefore patients undergoing cataract surgery should be informed of these limitations of ultrasonography.
We were able to diagnose multiple pathologies in cataract patients by B-Scan which can assist the surgeon regarding the operative and post operative management of the cataract patients. However, a large study with larger sample size is required to evaluate the B-Scan as a preoperative diagnostic modality in cataract patients and to evaluate complete spectrum of pathologies related to posterior segment.
Conclusion
B-scan is a good diagnostic modality for preoperative evaluation of posterior segment pathologies in the presence of cataract.
References
- Murthy GV, Guptha SK, John N, Vashist P (2008) Current status of cataract blindness and Vision 2020: The right to sight initiative in India. Indian J Ophthalmol 56: 489-494.
- Mendes MH, Betinjane AJ, Cavalcante Ade S, Cheng CT, Kara-José N (2009) Ultrasonographic findings in patients examined in cataract detection-and- treatment campaigns: a retrospective study. Clinics (Sao Paulo) 64: 637-640.
- Salman A, Parmar P, Vanila CG, Thomas PA, Jesudasan CA (2006) Is ultrasound essential before surgery in eyes with advanced cataracts? J Postgraduate Med 52: 19-22.
- Perry LJ (2012) The evaluation of patients with traumatic cataracts by ultrasound technologies. Semin Ophthalmol 27: 121-124.
- Qureshi MA, Laghari K (2010) Role of B-scan ultrasonography in pre-operative cataract patients. Int J Health Sci (Qassim) 4: 31-37.
- Mundt GH Jr, Hughes WF Jr (1956) Ultrasonics in ocular diagnosis. Am J Ophthalmol 41: 488-498.
- Baum G, Greenwood I (1958) The application of ultrasonic locating techniques to ophthalmology. II. Ultrasonic slit lamp in the ultrasonic visualization of soft tissues. AMA Arch Ophthalmol 60: 263-279.
- Bronson NR 2nd, Turner FT (1973) A simple B-scan ultrasonoscope. Arch Ophthalmol 90: 237-238.
- Anteby II, Blumenthal EZ, Zamir E, Waindim P (1998) The role of preoperative ultrasonography for patients with dense cataract: a retrospective study of 509 cases. Ophthalmic Surg Lasers 29: 114-118.
- Kalpna BN, Murali B (2015) Cataract and posterior segment risk factors. Med Res Chron 2: 226-234.
- Chanchlani M, Chanchlani R (2016) A study of posterior segment evaluation by B-Scan in hyper mature cataract. J Clin Exp Ophthalmol 7: 516.